Unit 4: The Practice of Longevity Coaching¶
Chapter 4.22: Integration & Prioritization¶
[CHONK: 1-minute summary]
What you'll learn in this chapter:
- How to apply the "Hierarchy of Longevity Needs" to prioritize interventions for any client
- Why the Adherence Paradox means simpler protocols often win long-term
- How to prevent "majoring in the minor" syndrome in clients seeking longevity coaching
- How to build personalized 12-month coaching roadmaps based on client assessment
- How to use the "Longevity Basics Audit" to identify where each client needs to start
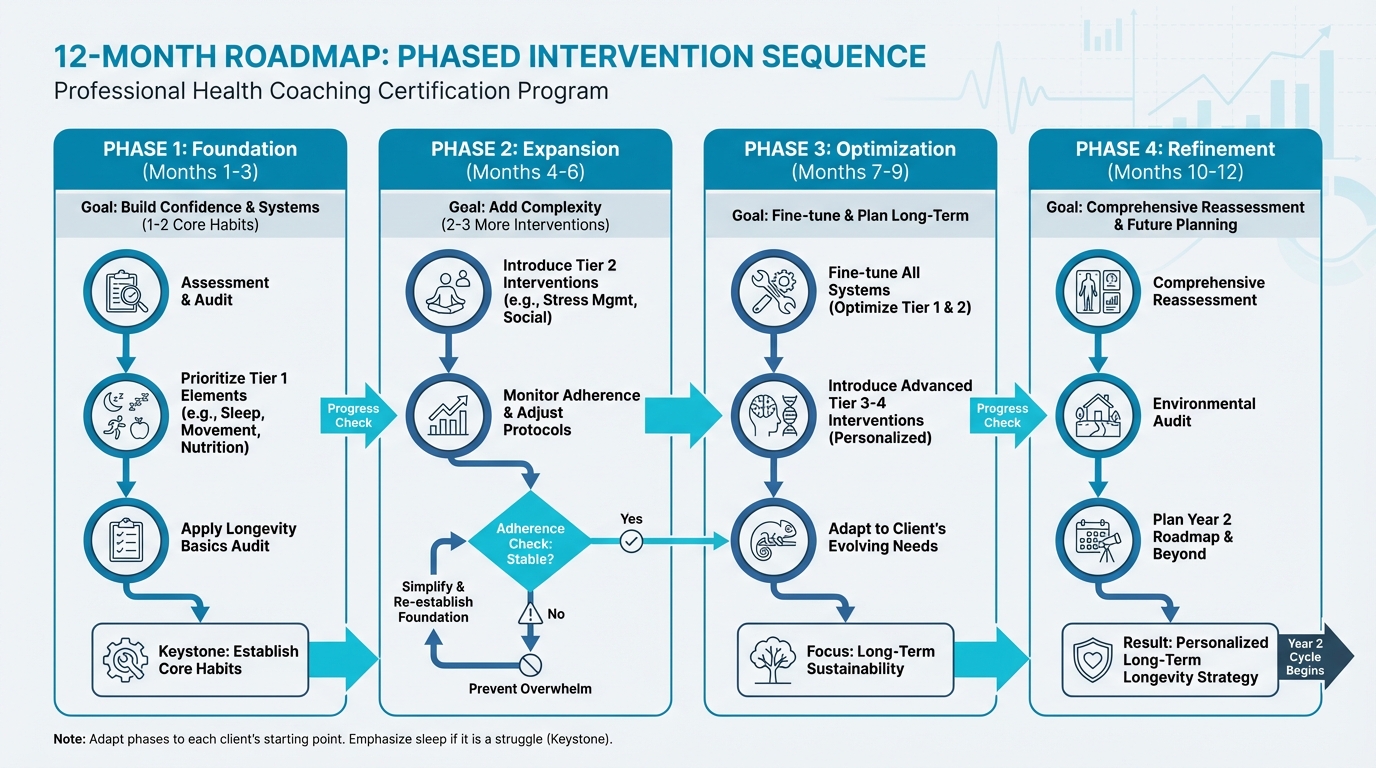
Figure: Phased intervention sequence
The big idea: Your clients have heard about cold plunges, sauna protocols, NMN supplements, and continuous glucose monitors. They've absorbed countless podcast hours on optimization. And many of them are doing all of this while getting five hours of sleep and eating takeout six nights a week. This chapter gives you the framework to help them focus on what actually matters. The interventions with the biggest impact come before chasing marginal gains. The research is clear: 80 percent adherence to a good protocol beats 40 percent adherence to a perfect one. Here's how to put that into practice.
[CHONK: Introduction - Don't Biohack Before You Sleep]
Don't Biohack Before You Sleep¶
Picture this client: James is a 45-year-old tech entrepreneur. He takes 23 supplements each morning. He owns a $6,000 cold plunge. He tracks his glucose continuously. He's experimented with rapamycin. He can quote Peter Attia's VO2 max recommendations by heart.
He also sleeps five hours a night, hasn't lifted weights in three years, and his social life consists primarily of Slack messages.
James isn't unusual. He's the archetype of a certain kind of longevity seeker, obsessed with optimizing the margins while the foundation crumbles beneath him.
The Optimization Paradox¶
Here's the uncomfortable truth about longevity optimization: the most exciting interventions are usually the least impactful.
Cold exposure, sauna protocols, exotic supplements, continuous glucose monitoring. These capture attention because they feel cutting-edge, scientific, controllable. They offer the seductive promise that we can hack our way to a longer life.
But the research tells a different story.
The interventions with the largest effect sizes on mortality and healthspan are the ones your grandmother could have told you about: sleep, movement, eating well, maintaining relationships, not smoking, limiting alcohol. These "boring" basics account for the vast majority of longevity outcomes. Roughly 70 percent or more, according to the best available evidence (1, 2, 3).
Everything else—the biohacks, the supplements, the advanced protocols—falls into the remaining 30 percent, and most of those interventions deliver effects measured in single-digit percentages.
This creates a paradox: clients are drawn to longevity coaching precisely because they want the advanced stuff, but what most of them actually need is help with the basics.
Why This Chapter Matters¶
In Chapter 1.6, you learned the PN 6-step coaching process adapted for longevity and how to assess, understand, strategize, choose, observe, and analyze over multi-year timeframes. You learned about the 3-month phased onboarding and multi-year roadmaps.
This chapter answers a different question: What should you prioritize?
Chapter 1.6 gave you the process. This chapter gives you the hierarchy.
By the end of this chapter, you'll have:
- A clear framework for sequencing interventions (the Hierarchy of Longevity Needs)
- Specific criteria for identifying "Non-Negotiables"
- Tools for recognizing and addressing "majoring in the minor" syndrome
- A practical audit checklist to identify where each client should start
- Coaching language and dialogues for redirecting clients toward what matters
Let's start with the hierarchy.
[CHONK: The Hierarchy of Longevity Needs]
The Hierarchy of Longevity Needs¶
Think of longevity interventions like a pyramid. The base is wide and stable: foundational interventions that almost everyone needs and that deliver the largest effects. As you move up, the pyramid narrows. Each level builds on the one below, and each level contributes less to overall outcomes.
The Four Tiers¶
Tier 1 (Foundation): ~70% of outcomes
These are the Non-Negotiables: the interventions that deliver the largest mortality reductions and that almost everyone should prioritize first.
- Sleep: 7-9 hours consistently
- Movement: 150+ minutes of physical activity weekly, including strength training
- Basic Nutrition: Adequate protein (target: 30g+ per meal), vegetables, minimally processed foods
- Social Connection: Regular meaningful contact with friends, family, community
- Health Basics: Annual comprehensive bloodwork, no smoking, alcohol within limits
The effect sizes here are substantial. Meeting physical activity guidelines is associated with 20-40 percent reductions in all-cause mortality (4). Each additional 1,000 steps per day is associated with roughly 9 percent lower mortality risk (5). Short sleep (under 7 hours) is associated with 14 percent higher mortality; long sleep (over 9 hours) with 34 percent higher mortality compared to 7-8 hours (6). Social isolation is associated with 32 percent higher mortality, comparable to smoking (7).
Tier 2 (Significant): ~20% of outcomes
These interventions matter, but they require Tier 1 to be in place first.
- Stress Management: Structured practices (meditation, breathwork, nature exposure)
- Environment Optimization: Reducing toxin exposure, improving air quality, optimizing light exposure
- Advanced Nutrition: Mediterranean/MIND diet principles, nutrient timing, blood sugar management
Improving diet quality over 12 years is associated with 8-17 percent lower mortality risk, depending on the index used (8). But these gains build on the foundation. Optimizing nutrient timing while sleeping five hours is unlikely to move the needle.
Tier 3 (Minor): ~9% of outcomes
These are meaningful interventions for clients with Tiers 1-2 solid.
- Supplements: Core supplements (vitamin D, omega-3, magnesium, creatine)
- Recovery Protocols: Sauna, cold exposure, structured recovery
- Testing Optimization: VO2 max testing, biological age clocks, advanced biomarkers
Sauna use (4+ sessions weekly) is associated with roughly 40 percent lower cardiovascular mortality in observational studies (9), but this is in populations who presumably also have other healthy behaviors in place. These aren't substitutes for the basics.
Tier 4 (Marginal): ~1% of outcomes
These are for clients who have everything else dialed in.
- Biohacks: Experimental interventions, precision optimization
- Advanced Testing: Continuous glucose monitoring (for non-diabetics), comprehensive genetics
- Cutting-Edge Protocols: Rapamycin, hyperbaric oxygen, peptides
The evidence here is thin, often extrapolated from animal studies or based on mechanistic reasoning rather than human mortality data. For the client who sleeps poorly, these are distractions.
The Graphic: Hierarchy of Longevity Needs¶
Visual concept: Pyramid structure with 4 tiers, wide at base, narrow at top
Tier 1 (Base - 70% width)
- Label: "Foundation: ~70% of outcomes"
- Color: Deep blue (PN primary #068FB9)
- Contents:
- Sleep (7-9 hours)
- Movement (150+ min/week)
- Basic Nutrition (protein, vegetables)
- Social Connection
- Health Basics (bloodwork, no smoking)
- Tagline: "If you do nothing else, do these"
Tier 2 (Middle-lower - 50% width)
- Label: "Significant: ~20% of outcomes"
- Color: Medium blue (#0D6782)
- Contents:
- Stress Management
- Environment Optimization
- Advanced Nutrition
- Tagline: "Build on the foundation"
Tier 3 (Middle-upper - 30% width)
- Label: "Minor: ~9% of outcomes"
- Color: Light blue (#00bbe3)
- Contents:
- Supplements
- Recovery Protocols (sauna, cold)
- Testing Optimization
- Tagline: "Worth doing after Tiers 1-2 are solid"
Tier 4 (Top - 10% width)
- Label: "Marginal: ~1% of outcomes"
- Color: Lightest blue/gray
- Contents:
- Biohacks
- Experimental Interventions
- Precision Optimization
- Tagline: "For those with everything else dialed in"
Side annotation: Arrow pointing to Tier 3-4 with text "Where many longevity seekers focus" contrasted with "Where most outcomes come from" pointing to Tier 1
Deep Health Across the Hierarchy¶
Notice how the hierarchy maps to all six Deep Health dimensions:
| Dimension | Tier 1 | Tiers 2-4 |
|---|---|---|
| Physical | Sleep, movement, nutrition | Testing, supplements, recovery |
| Emotional | Social connection | Stress management |
| Mental | Sleep (cognitive function) | Cognitive training, advanced protocols |
| Social | Relationships, community | |
| Environmental | Environment optimization | |
| Existential | Purpose sustaining habits | Long-term planning |
The foundation (Tier 1) touches multiple dimensions simultaneously. Sleep affects physical health, cognitive function, and emotional regulation. Social connection supports emotional health and provides accountability for physical health behaviors. Movement improves mood, cognition, and physical markers.
This is why Tier 1 delivers such outsized returns: these interventions create positive cascades across dimensions.
[CHONK: The Non-Negotiables]
The Non-Negotiables: What Actually Moves the Needle¶
The longevity protocol (referenced throughout this course) identifies six "Non-Negotiables": interventions that deliver the largest effects and that should be prioritized before anything else:
If you do nothing else, do these:
- 150 min of exercise weekly (strength & cardiovascular)
- Sleep 7-9 hours consistently
- Eat adequate protein (30 grams per meal target)
- Maintain strong relationships/social connections
- Get annual comprehensive bloodwork
- Don't smoke/excessive drinking
Let's look at the evidence behind each.
Exercise: The Most Powerful Longevity Drug¶
Exercise produces larger mortality reductions than any other lifestyle intervention, and possibly larger than most medications.
Meeting aerobic activity guidelines (approximately 150 minutes per week of moderate activity) is associated with substantially lower all-cause mortality across ages (4). The benefits are often greater in older adults than younger adults, meaning it's never too late.
But here's what's often missed: cardiorespiratory fitness is even more predictive than exercise volume alone. High cardiorespiratory fitness is associated with roughly 47 percent lower cancer mortality compared to low fitness (10). VO2 max is one of the strongest predictors of all-cause mortality we have. Stronger than most biomarkers.
What this means for your client: Start with any movement. 150 minutes weekly is the minimum target. But help clients progress toward including both strength training (for muscle mass, bone density, and functional capacity) and cardiovascular training (for VO2 max and metabolic health). The combination matters.
Sleep: The Foundation of Everything Else¶
Sleep follows a U-shaped relationship with mortality. Both short and long sleep carry elevated risk.
A 2025 meta-analysis pooling data from 79 prospective cohorts found (6):
- Short sleep (<7 hours): 14 percent higher all-cause mortality
- Long sleep (≥9 hours): 34 percent higher all-cause mortality
- Optimal: 7-8 hours consistently
Sleep isn't just about duration. Sleep is an active metabolic process. During sleep, the glymphatic system, the brain's waste-clearance system, removes beta-amyloid plaques (protein buildups associated with Alzheimer's disease). Growth hormone is released, and memory is consolidated.
What this means for your client: Sleep is foundational. It affects every other intervention's effectiveness. A client who optimizes nutrition but sleeps five hours is fighting with one hand tied behind their back. Prioritize sleep optimization early in the coaching relationship.
Nutrition: Adequate Protein and Vegetables¶
Diet quality improvements are associated with meaningful mortality reductions, though typically smaller than exercise or sleep.
Improving diet quality over 12 years (measured by validated indices like the AHEI—Alternative Healthy Eating Index—Mediterranean, or DASH score) is associated with 8-17 percent lower all-cause mortality (8). Plant-forward macronutrient profiles are associated with modestly lower mortality, while higher animal fat intake is associated with modestly higher mortality (11).
But notice: the effect sizes for diet are smaller than for exercise or sleep. This doesn't mean nutrition doesn't matter. It means adequate is more important than optimal for most clients.
What this means for your client: Don't let perfect be the enemy of good. Focus on adequate protein (30g+ per meal supports muscle protein synthesis), vegetables (6-10 servings daily), minimally processed foods, and limiting alcohol. Once these basics are solid, refinement becomes more valuable.
Social Connection: As Important as Not Smoking¶
Social isolation is associated with 32 percent higher all-cause mortality. Loneliness is associated with 14 percent higher mortality (7). These effect sizes are comparable to well-established risk factors like smoking.
Social connection appears to work through multiple pathways: reduced stress, improved immune function, better health behaviors (accountability), and greater meaning/purpose.
What this means for your client: Social connection isn't a nice-to-have. It's a Non-Negotiable. For isolated clients, building social connection may be as important as exercise or nutrition interventions.
Health Basics: Screening and Harm Reduction¶
Annual comprehensive bloodwork allows early detection of metabolic dysfunction, inflammation, and disease risk. This isn't about optimization. It's about catching problems early when they're most treatable.
And the harm reduction basics: not smoking produces the largest single-behavior effect on life expectancy (12). Limiting alcohol to 2-4 drinks per week maximum aligns with current evidence on cardiovascular and cancer risk.
What this means for your client: Ensure clients are getting annual bloodwork and staying within scope (Chapter 1.5) when interpreting results. For clients who smoke, cessation may be the single highest-impact intervention: larger than any supplement or biohack.
Coaching in Practice: The Supplement-Obsessed Client¶
[CHONK: Coaching in Practice - The Supplement-Obsessed Client]
Your client Marcus, 48, asks about NMN dosing, berberine timing, and whether he should add metformin. He takes 15 supplements daily and spends $400/month on them.
Before diving into his supplement questions, you explore his basics:
- "How's your sleep these days?" (5-6 hours, irregular)
- "What does a typical week of exercise look like?" (Walking the dog, occasional weekend hike)
- "Tell me about your protein intake." (Skips breakfast, light lunch, larger dinner)
Without judging his supplement interest, you help him see the hierarchy: "I appreciate your commitment to optimizing. That's exactly the mindset we need. Let me share something interesting: the research suggests that sleep and consistent exercise deliver 10-20x the mortality reduction of even the best supplements. Before we fine-tune your stack, what if we got your sleep to 7-8 hours and built a consistent strength training habit? Then those supplements would work even better on a stronger foundation."
Key takeaway: The goal isn't to dismiss his interests. It's to sequence them appropriately.
The 80/20 of Longevity¶
The Pareto principle (80/20 rule) applies to health interventions. Research on healthcare spending shows that roughly 80 percent of spending is incurred by roughly 20 percent of patients (13). Analysis of global health interventions shows that the top quartile of interventions delivers roughly 79 DALYs (disability-adjusted life years) averted per $1,000, compared to a median of about 5 DALYs/$1,000 (14).
The top ~2.5 percent most cost-effective interventions deliver 25-38 times the median impact.
In practical terms: a small number of interventions deliver the vast majority of results. The Non-Negotiables are those high-leverage interventions for longevity.
[CHONK: Building the 12-Month Roadmap]
Building the 12-Month Roadmap¶
In Chapter 1.6, you learned about the 3-month phased onboarding strategy (Month 1: Foundation, Month 2: Expansion, Month 3: Optimization) and multi-year roadmaps. This section shows you how to apply that framework specifically to the hierarchy of needs.
The Protocol's Phased Approach¶
The longevity protocol recommends a systematic build:
Don't try to implement everything at once. Build systematically.
Month 1: Foundation
- Sleep optimization
- Strength training 3x/week
- Protein targets
- Core supplements (if necessary)
- Consider HRT (if appropriate)
- Baseline testing (bloodwork, DEXA, VO2 max)
Month 2: Expansion
- Add Zone 2 cardio
- Introduce sauna/cold
- Refine nutrition
- Social connection focus
- Refine stress management practices
Month 3: Optimization
- VO2 max training
- Full supplement stack
- Environmental audit
- Biomarker testing
Ongoing: Refinement
- Quarterly assessments
- Protocol adjustments
- Continuous education
- Community building
Adapting the Phases to Each Client¶
These phases are guidelines, not rigid prescriptions. The specifics depend on where each client starts.
If your client already exercises consistently:
- Month 1 might focus on sleep optimization and nutrition refinement
- You can introduce Zone 2 and strength progression earlier
- The foundation phase might be shorter
If your client struggles with sleep:
- Month 1 should heavily emphasize sleep hygiene and consistency
- Don't add too many other interventions that could overwhelm
- Sleep is the keystone. Get this right first
If your client is socially isolated:
- Social connection might be the primary Month 1 focus
- Consider social forms of exercise (group classes, walking partners)
- Build the social foundation alongside physical foundations
If your client has existing health conditions:
- Coordinate with healthcare providers (scope of practice, Chapter 1.5)
- Prioritize interventions that support medical treatment
- Be conservative with adding complexity
Research on Phased vs. All-at-Once Implementation¶
The research generally supports phased approaches, though with nuance.
A head-to-head trial comparing sequential (one behavior at a time) versus simultaneous (multiple behaviors at once) delivery found (15):
- At 12 months, sequential approaches showed larger overall risk reduction
- At 24 months, simultaneous approaches caught up or exceeded
- Sequential approaches achieved higher smoking abstinence at both timepoints
Another trial found that starting with diet could temporarily suppress increases in physical activity, while exercise-first yielded early PA gains (16). By 12 months, all groups improved. The path mattered for early momentum.
Key insight: Phased implementation isn't always superior, but it reduces overwhelm, builds confidence through early wins, and is more sustainable for most clients. The WHO reports that only about 50 percent of patients with chronic conditions adhere to long-term therapies in developed countries (17). Simpler is often more sustainable.
What this means for your client: Start with 1-2 interventions in Month 1. Build confidence and systems before adding complexity. Monitor adherence. If it's dropping, you've added too much too fast.
Coaching in Practice: Sample 12-Month Roadmap¶
[CHONK: Coaching in Practice - Sample 12-Month Roadmap]
Client profile: Elena, 52, busy executive. Sleep: 5-6 hours. Exercise: occasional yoga. Nutrition: skips breakfast, late dinners. Social: strong family, limited friends. VO2 max: 28 (below target of 35+).
Month 1: Foundation
- Primary focus: Sleep (target 7 hours, consistent bedtime)
- Secondary: Daily 10-minute walk (building movement habit)
- Assessment: Baseline bloodwork, establish Deep Health baseline
Month 2: Expansion
- Continue sleep optimization (target 7.5 hours)
- Add strength training 2x/week (compound movements)
- Begin protein focus (30g at breakfast and lunch)
Month 3: Optimization
- Maintain sleep, continue strength training
- Add Zone 2 cardio 2x/week (building toward 150 min total)
- Refine nutrition (Mediterranean principles)
Months 4-6: Building
- Progress strength training to 3x/week
- Increase Zone 2 toward 150+ minutes weekly
- Social focus: reconnect with old friends (1 coffee date/week)
Months 7-9: Deepening
- Introduce stress management practices
- Consider core supplements if gaps exist
- Retest VO2 max (target: improvement to 30+)
Months 10-12: Refinement
- Fine-tune all systems
- Environmental audit
- Plan Year 2 roadmap
- Comprehensive reassessment
Key takeaway: Notice that sauna, cold exposure, and optimization protocols don't appear until the foundation is solid, if at all in Year 1. Elena's gaps are in Tier 1; Tier 3 can wait. |
[CHONK: The Adherence Paradox]
The Adherence Paradox¶
Here's the counterintuitive truth at the heart of longevity coaching:
80% adherence to a good protocol beats 40% adherence to a perfect protocol.
This is the Adherence Paradox. The more complex and "optimized" a protocol becomes, the harder it is to sustain, and unsustainable protocols fail, no matter how scientifically sound they are.
Why Simpler Wins Long-Term¶
Cognitive load matters. Tracking 15 supplements, timing meals around workouts, monitoring glucose, optimizing sleep hygiene, maintaining a complex strength program. Each intervention consumes mental bandwidth. Eventually, something gives.
A 2021 study found that overly customized feedback in a physical activity app actually reduced user engagement. More personalization wasn't better (18). There's a complexity-adherence trade-off: too much optimization backfires.
Willpower is finite. Behavior change research consistently shows that habit formation takes sustained effort: median time to automaticity is 59-66 days, with individual ranges from 4 to 335 days (19). During that formation period, you're drawing on limited self-regulatory resources. The more behaviors you're trying to establish simultaneously, the more you deplete those resources.
Competing demands are real. Your clients have jobs, families, responsibilities. A protocol designed for a professional athlete with 20 hours weekly to devote to health optimization isn't realistic for a busy executive or a parent of young children. The "perfect" protocol that doesn't fit their life will be abandoned.
Research on the Adherence Paradox¶
A trial in prediabetic adults tested whether augmenting or re-sequencing program components for slow responders would improve outcomes. The result? No long-term advantage from augmentation or re-sequencing, and the augmented sequence actually reduced self-efficacy (20).
Adding complexity didn't help. It may have made things worse by undermining clients' confidence.
Health coaching meta-analyses show small-to-moderate improvements in quality of life, self-efficacy, and outcomes, with effect sizes around 0.3-0.6 (21). These aren't dramatic transformations. They're sustainable, meaningful improvements built on realistic protocols.
Practical Applications¶
Start simpler than you think necessary. If your instinct is to give a client three interventions, try two. If you're tempted to add a fourth supplement, wait. Build confidence and systems before adding complexity.
Track adherence, not just outcomes. A client who "fails" at a complex protocol may succeed at a simpler one. The failure isn't the client. It's the protocol-client mismatch. Ask regularly: "What percentage of the time are you doing this?" Anything below 70-80 percent signals the need to simplify.
Celebrate sustainable wins. A client who walks 20 minutes daily for 6 months has achieved more than a client who did intense workouts for 3 weeks before burning out. Help clients see that consistency trumps intensity.
[CHONK: "Majoring in the Minor" Prevention]
"Majoring in the Minor" Prevention¶
"Majoring in the minor" is a common failure mode in longevity-focused clients. They obsess over marginal optimizations while neglecting foundational behaviors.
Recognizing the Pattern¶
The Cold Plunge Obsession
Your client has a $5,000 cold plunge in their garage. They follow precise Huberman protocols: 2-3 minutes at 50°F, four times weekly. They can cite the research on dopamine and norepinephrine increases.
They also sleep 5 hours a night and haven't done strength training in years.
Cold exposure may offer benefits for resilience and metabolic health. But the effect sizes are modest, and most evidence comes from small studies. Sleep deprivation, meanwhile, is associated with 14-34 percent increased mortality risk. The hierarchy is clear.
The Supplement Stack
Your client spends $500/month on supplements: NMN, berberine, sulforaphane, CoQ10, a dozen others. They've researched each one carefully.
They also skip vegetables, rarely hit protein targets, and haven't had bloodwork in three years.
Even the best supplements deliver marginal effects compared to adequate nutrition. And without bloodwork, you don't know what deficiencies (if any) actually exist.
The Sauna Maximizer
Your client does sauna 5 times weekly, following the Finnish studies showing cardiovascular benefits. They've optimized temperature and duration.
They also struggle to fit in two strength training sessions weekly.
Sauna is a Tier 3 intervention. Strength training is Tier 1. The hierarchy matters.
The "Basics Audit" Framework¶
When you suspect a client is majoring in the minor, use the Longevity Basics Audit. This checklist (included below) assesses whether Tier 1 fundamentals are in place before Tier 2-4 optimizations.
The principle: Don't optimize what isn't yet adequate.
The Longevity Basics Audit Checklist¶
Use this checklist to assess whether your client has fundamentals in place before adding optimizations. This complements the Deep Health Assessment from Chapter 1.3.
Tier 1: Non-Negotiables (Check all that apply)
Sleep
- [ ] Consistently sleeping 7-9 hours per night
- [ ] Regular sleep/wake schedule (±30 minutes)
- [ ] No undiagnosed sleep disorders
Movement
- [ ] 150+ minutes of physical activity weekly
- [ ] Includes some strength training (2+ sessions/week)
- [ ] Includes some cardiovascular training
Nutrition
- [ ] Eating adequate protein (target: 30g+ per meal)
- [ ] Regular vegetable consumption (5+ servings daily)
- [ ] Minimal ultra-processed food intake
Social Connection
- [ ] Regular meaningful contact with friends/family
- [ ] Not socially isolated
- [ ] Sense of belonging to community
Health Basics
- [ ] Annual comprehensive bloodwork
- [ ] No smoking
- [ ] Alcohol within recommended limits (≤2-4 drinks/week)
Scoring
- 10-12 checked: Foundation solid. Ready for Tier 2-3 optimizations
- 6-9 checked: Foundation needs work. Prioritize unchecked items before optimizing
- 0-5 checked: Foundation critical. Focus exclusively on Tier 1 until 8+ items checked
Connection to Deep Health Assessment
Map results to your client's Deep Health Assessment (Chapter 1.3):
- Sleep gaps → Physical and Mental dimensions
- Movement gaps → Physical and Emotional dimensions
- Nutrition gaps → Physical dimension
- Social gaps → Social/Relational and Emotional dimensions
- Health basics gaps → Physical dimension
Use both assessments together to identify WHERE to start with each client.
Coaching Conversations for Redirection¶
When redirecting a client away from optimization and toward foundations, use curiosity rather than dismissal.
Coaching in Practice: Redirecting the Biohacker¶
[CHONK: Coaching in Practice - Redirecting the Biohacker]
Client: "I've been researching rapamycin. What do you think about adding it to my protocol?"
Instead of: "That's too advanced for you" or "You're not ready for that"
Try: "I appreciate you doing that research. It shows real commitment. Before we explore rapamycin, I'm curious: how are the foundations going? Tell me about your sleep this past week."
(Client reveals sleep is 5-6 hours, inconsistent)
Coach: "Here's what's interesting. Rapamycin is being studied for longevity, but the effect sizes in humans are still uncertain. Sleep, on the other hand, has massive, well-established effects on every system we care about. What if we got your sleep dialed in first? Then, if you're still interested in rapamycin in 6 months, we could explore it from a much stronger foundation."
Key takeaway: Acknowledge their interest, share the hierarchy logic, and redirect without judgment. They're not wrong to be curious. They're just sequencing incorrectly. |
When Optimization Obsession Signals Something Deeper¶
Sometimes "majoring in the minor" isn't just a sequencing error. It's a sign of something deeper.
Health anxiety can drive obsessive optimization. The client who needs to control every variable may be managing underlying anxiety about mortality, aging, or control. This is beyond coaching scope but worth recognizing (Chapter 1.5). If you suspect clinical anxiety, refer appropriately.
Perfectionism can manifest as never-good-enough optimization. No matter how much the client does, there's always something more to add. This client may benefit from exploring identity and values (covered more in Chapter 26) rather than adding more interventions.
Avoidance can hide behind complexity. A client focused on obscure supplements may be avoiding harder changes, like quitting alcohol or addressing relationship issues. The advanced stuff is interesting; the basics are uncomfortable.
In these cases, the issue isn't information about the hierarchy. It's the underlying psychology. Use your coaching skills to explore what's driving the behavior.
[CHONK: Adapting the Framework to Each Client]
Adapting the Framework to Each Client¶
The hierarchy provides structure. But every client is different. Your job is to apply the framework to each individual's situation, starting point, and context.
How to Adjust Based on Client Starting Point¶
The client who already exercises consistently
If movement is solid, don't belabor it. Assess the other Tier 1 areas: Is sleep optimized? Is protein adequate? Are social connections strong? Start where the gaps are, not where you have a standard protocol.
The excellent sleeper who doesn't move
Great. They have one foundation in place. Build on it by linking movement to their sleep habits. "Since you're already protecting your sleep, what if we added a morning walk? Research shows morning movement can reinforce your circadian rhythm and improve sleep quality even further."
The socially isolated client
Don't ignore this because it's "soft." Social isolation has effect sizes comparable to smoking. For this client, social connection might be the primary Month 1 focus. Consider:
- Group fitness classes (movement + social)
- Walking with a friend (movement + social)
- Community involvement aligned with their values
The client with excellent fundamentals
They exist. For clients with sleep, movement, nutrition, and social connection dialed in, you can move to Tier 2-3 more quickly. These clients may legitimately be ready for supplement optimization, recovery protocols, and advanced testing. Apply the hierarchy, but recognize when someone is genuinely at a higher tier.
Using Deep Health to Identify Gaps¶
The Deep Health Assessment (Chapter 1.3) provides a multidimensional view. Use it alongside the Longevity Basics Audit to identify where each client needs to start.
Example mappings:
| Deep Health Gap | Likely Longevity Priority |
|---|---|
| Physical low, others high | Focus on movement, sleep, nutrition basics |
| Emotional low | Stress management, sleep (affects emotion regulation), social connection |
| Social/Relational low | Social connection: this IS a Tier 1 priority |
| Mental/Cognitive low | Sleep (affects cognition), movement (neurogenesis), stress management |
| Environmental low | Tier 2 environmental optimization, but only after Tier 1 is solid |
| Existential low | Purpose work: this sustains long-term adherence |
"This Is a Guide, Not a Prescription"¶
Throughout this chapter, we've presented frameworks, hierarchies, and checklists. These are tools, not mandates.
Longevity coaching is fundamentally client-led (Chapter 1.5). You guide, you don't prescribe. The client chooses their priorities based on their values, readiness, and life context. Your job is to:
- Help them see the hierarchy clearly
- Identify their specific gaps using assessments
- Offer informed recommendations based on evidence
- Let them lead on final decisions
A client who insists on starting with sauna before fixing their sleep isn't "wrong". They're making their own choice. Your role is to ensure they're making an informed choice, understanding the trade-offs. If they still choose the sauna, you work with them on that while gently continuing to highlight the sleep opportunity.
This is coaching, not prescribing.
[CHONK: Summary]
Summary¶
Longevity coaching success depends on prioritization. The interventions that capture attention, biohacks, exotic supplements, advanced protocols often deliver the smallest effects. The interventions that move the needle, sleep, movement, nutrition, social connection are foundational, not optional.
Key Takeaways¶
The Hierarchy of Longevity Needs:
- Tier 1 (Foundation): ~70% of outcomes → Sleep, movement, nutrition, social connection, health basics
- Tier 2 (Significant): ~20% of outcomes → Stress management, environment, advanced nutrition
- Tier 3 (Minor): ~9% of outcomes → Supplements, recovery protocols, testing
- Tier 4 (Marginal): ~1% of outcomes → Biohacks, experimental interventions
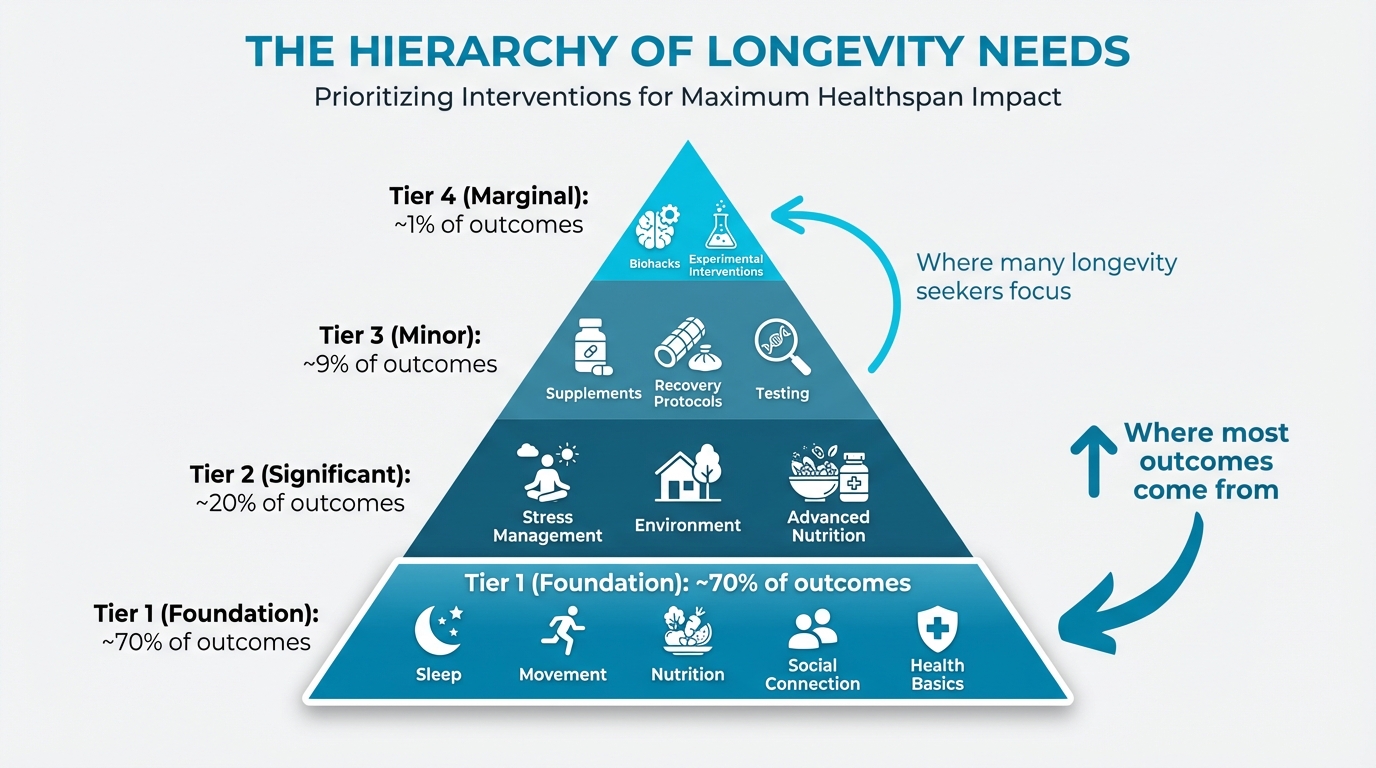
Figure: Tier 1/2/3 visual with % outcomes
The Non-Negotiables (if you do nothing else):
- 150+ minutes exercise weekly (strength + cardio)
- 7-9 hours sleep consistently
- Adequate protein (30g+ per meal)
- Strong social connections
- Annual bloodwork
- No smoking, limited alcohol
The Adherence Paradox:
- 80% adherence to good > 40% adherence to perfect
- Simpler protocols are more sustainable
- Complexity often backfires
- Start with less, build gradually
The Phased Approach:
- Month 1: Foundation (1-2 core habits)
- Month 2: Expansion (add 2-3 more)
- Month 3: Optimization (fine-tune, plan long-term)
- Adapt phases to each client's starting point
Preventing "Majoring in the Minor":
- Use the Longevity Basics Audit before adding optimizations
- Redirect with curiosity, not dismissal
- Recognize when optimization obsession signals deeper issues
- Don't optimize what isn't yet adequate
What's Coming Next¶
In Chapters 23-25, you'll apply this prioritization framework to detailed case studies: the stressed executive, the aging athlete, and the health-anxious optimizer. You'll see how the hierarchy translates to real coaching conversations and multi-year plans.
In Chapter 26, you'll go deeper on behavior change psychology and how to help clients shift their identity to sustain long-term change.
In Chapter 27, you'll learn about creating your longevity coaching practice, including the business and professional dimensions of this work.
For now, remember the core principle: Don't biohack before you sleep. Help your clients build the foundation first. Everything else becomes more effective when the basics are in place.
[CHONK: Study Guide Questions]
Study Guide Questions¶
Here are some questions that can help you think through the material and prepare for the chapter exam. They're optional, but we recommend you try answering at least a few as part of your active learning process.
-
What are the four tiers of the Hierarchy of Longevity Needs, and approximately what percentage of outcomes does each tier contribute?
-
List the six Non-Negotiables from the longevity protocol. Which has the strongest evidence for mortality reduction?
-
Explain the Adherence Paradox in your own words. Why does "80% adherence to good beat 40% adherence to perfect"?
-
A client asks about starting a complex supplement stack. They currently sleep 5-6 hours and don't exercise regularly. How would you respond using the concepts from this chapter?
-
What is "majoring in the minor" syndrome? Give two examples of how it might appear in a longevity-focused client.
-
How does the Longevity Basics Audit connect to the Deep Health Assessment from Chapter 1.3?
-
Describe how you would adapt the Month 1/2/3 phased approach for a client who already has excellent sleep habits but doesn't exercise.
-
A client scores 5/12 on the Longevity Basics Audit but wants to focus on sauna protocols and cold exposure. Using this chapter's principles, how would you approach this coaching conversation?
-
What role does social connection play in the Hierarchy of Longevity Needs? What effect size is associated with social isolation?
-
How do you balance the structured framework of the hierarchy with the PN principle that coaching should be client-led, not prescriptive?
Deep Dives¶
Want to go deeper? These supplemental articles explore key topics from this chapter in more detail.
- Hierarchy of Longevity Needs: Full breakdown of Tier 1-3 evidence with specific effect sizes
References¶
-
Lo W, Hu T, Shih C, Lin H, Hwang J. Impact of Healthy Lifestyle Factors on Life Expectancy and Lifetime Health Care Expenditure: Nationwide Cohort Study. JMIR Public Health and Surveillance. 2024;10:e57045. doi:10.2196/57045
-
Jackowska B, Wiśniewski P, Noiński T, Bandosz P. Effects of lifestyle-related risk factors on life expectancy: A comprehensive model for use in early prevention of premature mortality from noncommunicable diseases. PLOS ONE. 2024;19(3):e0298696. doi:10.1371/journal.pone.0298696
-
Todd B.. How much do solutions to social problems differ in their effectiveness?. 80,000 Hours; 2023. https://80000hours.org/2023/02/how-much-do-solutions-differ-in-effectiveness/
-
Martinez-Gomez D, Luo M, Huang Y, Rodríguez-Artalejo F, Ekelund U, Sotos-Prieto M, et al. Physical Activity and All-Cause Mortality by Age in 4 Multinational Megacohorts. JAMA Network Open. 2024;7(11):e2446802. doi:10.1001/jamanetworkopen.2024.46802
-
Eberth S, et al.. Daily steps and all-cause mortality: An umbrella review and meta-analysis. Prev Med; 2024. https://pubmed.ncbi.nlm.nih.gov/38901742/
-
Ungvari Z, Fekete M, Varga P, Fekete JT, Lehoczki A, Buda A, et al. Imbalanced sleep increases mortality risk by 14–34%: a meta-analysis. GeroScience. 2025;47(3):4545-4566. doi:10.1007/s11357-025-01592-y
-
Wang F, Gao Y, Han Z, Yu Y, Long Z, Jiang X, et al. A systematic review and meta-analysis of 90 cohort studies of social isolation, loneliness and mortality. Nature Human Behaviour. 2023;7(8):1307-1319. doi:10.1038/s41562-023-01617-6
-
Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, et al. Association of Changes in Diet Quality with Total and Cause-Specific Mortality. New England Journal of Medicine. 2017;377(2):143-153. doi:10.1056/nejmoa1613502
-
Laukkanen T, Khan H, Zaccardi F, Laukkanen JA. Association Between Sauna Bathing and Fatal Cardiovascular and All-Cause Mortality Events. JAMA Internal Medicine. 2015;175(4):542. doi:10.1001/jamainternmed.2014.8187
-
Dougherty TP, Meyer JE. Comparing Lifestyle Modifications and the Magnitude of Their Associated Benefit on Cancer Mortality. Nutrients. 2023;15(9):2038. doi:10.3390/nu15092038
-
Krakauer NY, Krakauer JC. Diet Composition, Anthropometrics, and Mortality Risk. International Journal of Environmental Research and Public Health. 2022;19(19):12885. doi:10.3390/ijerph191912885
-
BMC Public Health. Living healthier for longer: Comparative effects of three heart-healthy behaviors on life expectancy with and without cardiovascular disease. BMC Public Health; 2009. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-9-487
-
Academic Medicine. Where population health misses the mark: breaking the 80/20 rule. Academic Medicine; 2015. https://pubmed.ncbi.nlm.nih.gov/25551859/
-
Todd B. How much do solutions to social problems differ in their effectiveness? A collection of all the studies we could find. 80,000 Hours; 2023. https://80000hours.org/2023/02/how-much-do-solutions-differ-in-effectiveness/
-
Schulz DN, Kremers SP, Vandelanotte C, van Adrichem MJ, Schneider F, Candel MJ, et al. Effects of a Web-Based Tailored Multiple-Lifestyle Intervention for Adults: A Two-Year Randomized Controlled Trial Comparing Sequential and Simultaneous Delivery Modes. Journal of Medical Internet Research. 2014;16(1):e26. doi:10.2196/jmir.3094
-
King AC, Castro CM, Buman MP, Hekler EB, Urizar GG, Ahn DK. Behavioral Impacts of Sequentially versus Simultaneously Delivered Dietary Plus Physical Activity Interventions: the CALM Trial. Annals of Behavioral Medicine. 2013;46(2):157-168. doi:10.1007/s12160-013-9501-y
-
World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. WHO; 2003. https://apps.who.int/iris/handle/10665/42682
-
Zhu J, Dallal DH, Gray RC, Villareale J, Ontañón S, Forman EM, et al. Personalization Paradox in Behavior Change Apps. Proceedings of the ACM on Human-Computer Interaction. 2021;5(CSCW1):1-21. doi:10.1145/3449190
-
Singh B, Murphy A, Maher C, Smith AE. Time to Form a Habit: A Systematic Review and Meta-Analysis of Health Behaviour Habit Formation and Its Determinants. Healthcare. 2024;12(23):2488. doi:10.3390/healthcare12232488
-
Miller CK, King D, Nagaraja HN, Fujita K, Cheavens JS. Does intervention sequence impact self-regulatory and behavioral outcomes in an adaptive trial among adults with prediabetes?. Health Psychology and Behavioral Medicine. 2024;12(1). doi:10.1080/21642850.2024.2385490
-
Boehmer KR, Álvarez-Villalobos NA, Barakat S, de Leon-Gutierrez H, Ruiz-Hernandez FG, Elizondo-Omaña GG, et al. The impact of health and wellness coaching on patient-important outcomes in chronic illness care: A systematic review and meta-analysis. Patient Education and Counseling. 2023;117:107975. doi:10.1016/j.pec.2023.107975