Unit 3: Advanced Topics & Disease Prevention¶
Chapter 3.21: Hormone Health for Men¶
[CHONK: 1-minute summary]
What you'll learn in this chapter:
- What actually happens to testosterone as men age, and what doesn't
- Evidence-based lifestyle strategies that support healthy testosterone levels
- What coaches need to know about testosterone replacement therapy (TRT), educationally
- Why fertility implications matter and are often overlooked
- How to navigate the noise of TRT marketing and "bro science"
- Scope-safe ways to support male clients with hormone-related concerns
The big idea: Testosterone matters for men's health, but the conversation around it has become distorted by aggressive marketing and oversimplified solutions. As a coach, you can be an island of sanity in this noisy space. Your role is to support lifestyle strategies that genuinely influence testosterone—sleep, body composition, stress management, and exercise—while recognizing that testosterone replacement therapy is a medical decision that belongs between a man and his physician. This chapter gives you the knowledge to educate clients accurately, support them effectively, and know exactly when to refer.
Critical scope note: Coaches do not diagnose low testosterone, interpret lab results, or recommend for or against TRT. We educate, support lifestyle changes, and refer to appropriate medical providers. This chapter is educational. It equips you to be helpful without crossing into medicine.
If hormone talk feels a bit intimidating right now, that's understandable. You don't need to be an endocrinologist to use this chapter well; you'll just need a solid grasp of the big ideas and where your role begins and ends. (We'll walk through that together.)
[CHONK: Testosterone and Aging: The Reality]
Testosterone and Aging: What Actually Happens¶
Let's start with what testosterone actually is and what it does. Testosterone is the primary male sex hormone, though women have it too, in smaller amounts. In men, it's responsible for:
- Muscle mass and strength
- Bone density
- Fat distribution
- Sex drive and erectile function
- Mood and energy
- Red blood cell production
- Sperm production
It's important stuff. And yes, testosterone levels do decline with age. But the reality is a lot more complex than the marketing suggests.
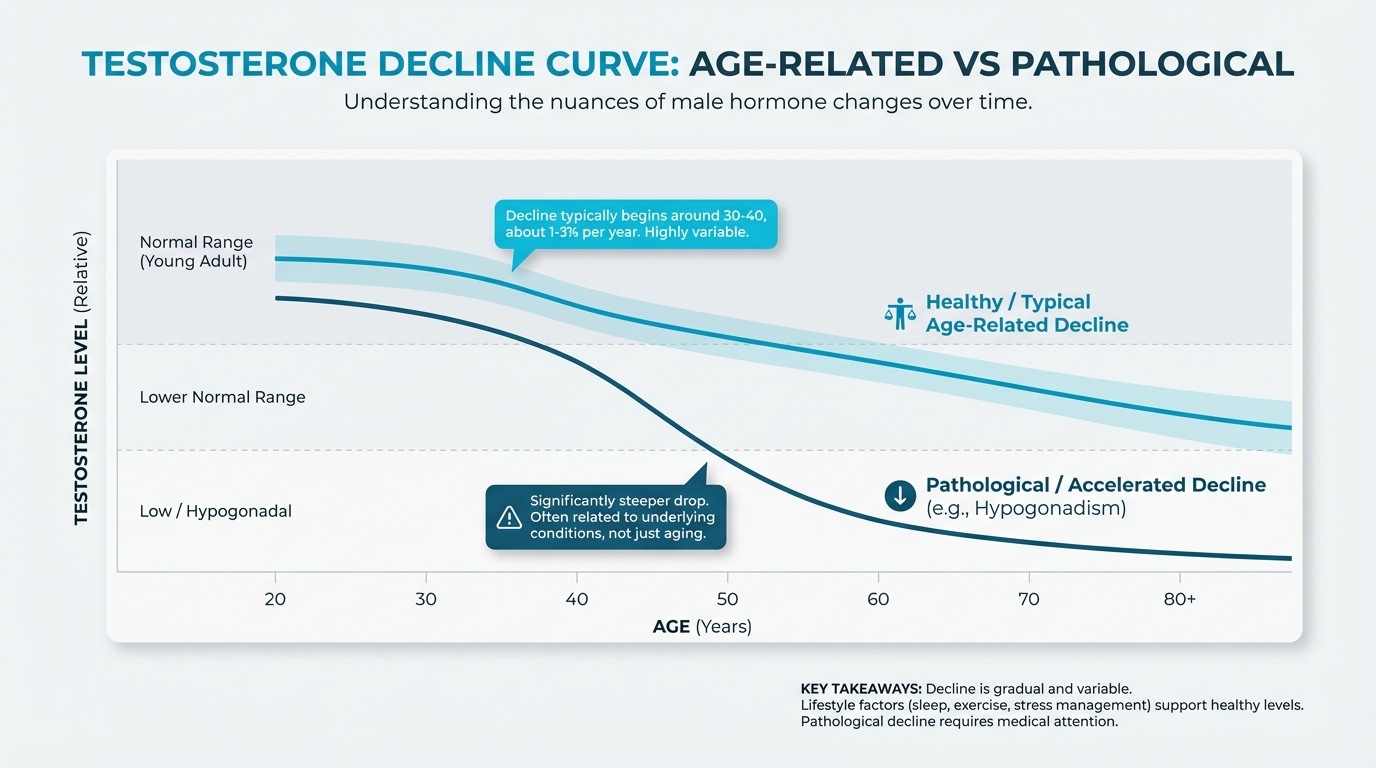
Figure: Age-related decline vs pathological
The Numbers on Decline¶
The research actually shows:
Testosterone typically begins declining around ages 30-40, with estimates ranging from about 1-3 percent per year. A 2024 review in Frontiers in Aging estimated approximately 2.8 percent annual decline in aging men.
But the key point is this: decline is gradual and highly variable. Some men maintain healthy testosterone levels well into their 70s and 80s. Others see significant drops earlier. By their 60s, only about 20 percent of men maintain total testosterone in the young-adult normal range. By their 80s, roughly half do.
If those numbers sound a bit discouraging or confusing, that's understandable. You don't need to memorize the exact percentages—the key idea is that change is gradual and highly individual.
This isn't menopause. Women experience an abrupt, universal loss of ovarian function at menopause. Men experience a slow, variable decline, more like a dimmer switch than an off button. This is why "andropause" or "male menopause" are misleading terms. The biology is fundamentally different.
What "Low Testosterone" Actually Means¶
This is where things get important for your coaching practice: low testosterone is a medical diagnosis, not something you or your client can determine from symptoms alone.
According to the Endocrine Society and American Urological Association guidelines, diagnosing hypogonadism (the medical term for abnormally low testosterone production) requires:
- Consistent symptoms of androgen deficiency (we'll cover these below)
- Unequivocally low morning testosterone confirmed on at least two separate occasions
- Use of reliable assays with standardized reference ranges
The commonly used threshold is total testosterone below 300 ng/dL (about 10.4 nmol/L), though there's variation across guidelines. The harmonized lower limit for young adult men is around 264 ng/dL.
If you're not used to thinking in lab cutoffs, don't worry. You don't need to recite these numbers to clients; you just need to remember that diagnosis requires both symptoms and properly timed, repeated testing.
Why morning testing matters: Testosterone follows a circadian rhythm. Levels are highest in the morning and decline throughout the day. Testing later in the day can give falsely low results.
Total T vs. Free T vs. SHBG¶
You'll hear clients mention these terms, so let's demystify them:
Total testosterone is everything in the blood: both testosterone that's bound to proteins and testosterone that's "free."
Free testosterone is the portion that's not bound to proteins. It's available to act on tissues. This represents only about 2-3 percent of total testosterone.
Sex hormone-binding globulin (SHBG) is a protein that binds testosterone, making it unavailable. As men age, SHBG typically increases, which means even if total testosterone stays the same, less of it is available to do its job.
If all these acronyms feel like alphabet soup, that's okay—you don't have to turn into a lab specialist to coach effectively.
This is why some men with "normal" total testosterone still experience symptoms. Their free testosterone may be low because SHBG is high. And it's why some guidelines recommend checking free testosterone when total testosterone is borderline (200-400 ng/dL).
What this means for your client: If a client brings up these terms, you can explain what they mean educationally. But interpreting whether their specific numbers are "good" or "bad"? That's for their physician. Your response: "That's a great question for your doctor. They can interpret what your specific numbers mean for you."
Symptoms of Low Testosterone¶
Men with genuinely low testosterone may experience:
- Reduced sex drive
- Erectile dysfunction
- Fatigue and low energy
- Decreased muscle mass and strength
- Increased body fat, especially around the midsection
- Mood changes (depression, irritability)
- Decreased bone density
- Hot flashes (yes, men can get these)
- Difficulty concentrating
The catch: Every single one of these symptoms can be caused by something other than low testosterone: poor sleep, stress, depression, obesity, medication side effects, or simply aging. This is why symptoms alone don't equal a diagnosis. It requires lab confirmation.
As a coach, you’re not expected to untangle all of those possible causes—that’s your client’s medical team’s job.
Why TRT Culture Oversimplifies¶
This is where we need to be honest about the environment your clients are navigating.
Testosterone prescriptions increased 10-fold in the United States and 40-fold in Canada over a single decade, without any new approvals for age-related use. That's not driven by an epidemic of genuine hypogonadism. It's driven by marketing.
Some clinics have lowered their thresholds for "low testosterone," diagnosing men who would be considered normal by major medical guidelines. Some promise benefits that the evidence doesn't support. Some minimize risks, particularly fertility risks.
Your job isn't to be anti-TRT. Testosterone replacement therapy is a legitimate medical treatment for men with genuine hypogonadism. Your job is to help clients separate evidence from hype, understand what lifestyle can and cannot do, and make sure they're having these conversations with qualified medical providers, and ensure they're not making decisions based on podcast claims or clinic marketing.
Coaching in practice: When a client says "I think my testosterone is low"¶
The scenario: Your client says, "I think my testosterone is low."
What NOT to do (out of scope): Jump in with, "Yeah, that sounds low. You should get your testosterone tested and probably go on TRT."
Why it doesn't work: That puts you in the role of diagnostician and prescriber, which is outside your scope.
What TO do instead: Stay curious, ask about context, and keep the focus on scope-safe next steps.
Sample dialogue:
Client: "I think my testosterone is low."
Coach: "I hear that you're concerned about your testosterone levels. What's making you think that? Are there specific symptoms you've noticed?"
Client: "I'm tired all the time and my sex drive is way down."
Coach: "Those are definitely things worth paying attention to. Low testosterone can be one cause, but so can sleep, stress, medications, and body composition. Low T is something that has to be confirmed with blood tests, ideally morning tests on two separate occasions."
Coach (scope-safe next step): "If this is worrying you, I'd suggest talking with your doctor or a urologist. They can do proper testing and figure out what's actually going on. In the meantime, there are lifestyle factors that can support healthy testosterone levels: sleep, strength training, managing stress, and maintaining a healthy body composition. We can absolutely work on those together."
Avoid saying: "Your testosterone is probably low." "You should get your levels checked." "Your numbers sound low to me." (You're not qualified to make these assessments.)
[CHONK: Supporting Healthy Testosterone Naturally (FIRST)]
Supporting Healthy Testosterone Through Lifestyle¶
Before we discuss TRT, which is a medical intervention, let's talk about what actually works to support healthy testosterone through lifestyle. This is your domain as a coach.
The honest truth is that lifestyle strategies can meaningfully influence testosterone levels, but they're not magic. They work best for men whose testosterone is being suppressed by modifiable factors like excess body fat, poor sleep, or chronic stress. They won't turn a man with genuine hypogonadism into a high-testosterone individual.
Let's look at the evidence for each strategy.
Body Composition: The Biggest Lever¶
If there's one lifestyle factor with the strongest evidence for influencing testosterone, it's body composition, specifically reducing excess body fat.
The research shows:
- A Mendelian randomization study (which provides causal evidence, not just correlation) found that each standard deviation increase in fat mass was associated with a 0.24 standard deviation decrease in total testosterone.
- Clinical reviews show that weight loss of 5-15 percent typically increases testosterone by 10-30 percent in men who are overweight or obese.
Why does fat matter? Adipose tissue (body fat) contains an enzyme called aromatase that converts testosterone to estrogen. More fat = more conversion = less testosterone available. Fat tissue also produces inflammatory compounds that can suppress testosterone production.
Visceral fat (the fat around internal organs, which shows up as a bigger waistline) may be particularly problematic, though some imaging studies find that total fat mass matters regardless of location.
What this means for your client: For overweight men concerned about testosterone, weight loss through sustainable calorie deficit and exercise is the most evidence-based intervention you can support. The good news: the same habits that support weight loss (strength training, adequate protein, better sleep, stress management) also support testosterone through other mechanisms.
Sleep: Protecting the Foundation¶
Sleep and testosterone are tightly linked, but the relationship is a bit more complex than it might sound.
What the research shows:
- Total sleep deprivation (24+ hours) substantially suppresses testosterone. Studies show large reductions (effect size around -0.67).
- Partial sleep restriction (like getting 5-6 hours instead of 7-8) shows less consistent effects in short-term studies. The pooled effect was not statistically significant in one meta-analysis.
- But population data from NHANES (8,748 adults) found that habitual sleep of 6 hours or less was associated with abnormal testosterone levels in men.
If keeping track of those details feels tricky, that's normal. The main idea is that chronically short, poor-quality sleep is much more concerning than the occasional late night.
The takeaway: Chronic short sleep likely matters more than occasional short nights. And the interventions that improve sleep quality (consistent sleep-wake times, dark room, managing stress) are things you can absolutely coach.
How to coach this: If a client is consistently getting under 6-7 hours and is concerned about testosterone, sleep improvement is a high-value target. You're not just addressing testosterone, you're addressing everything else sleep affects (recovery, mood, body composition, cognitive function).
Strength Training: Building the Infrastructure¶
One finding that surprises many people is that chronic exercise training, including resistance training, does not consistently increase resting testosterone levels in healthy or older men.
A meta-analysis of 11 randomized controlled trials (421 men) found that exercise training had essentially zero effect on resting total testosterone (effect size = 0.00). Another meta-analysis specifically in men over 60 found resistance training did not significantly change basal testosterone.
Wait, what? Didn't we all hear that lifting weights boosts testosterone?
The nuance is that exercise can produce transient, acute increases in testosterone, especially high-intensity work. And in some populations (like young athletes doing intensive training), sustained increases have been observed. But for the typical client? Exercise doesn't reliably raise their baseline testosterone levels.
Does that mean exercise doesn't matter? Absolutely not. Exercise matters enormously for:
- Building muscle mass (which supports metabolic health and body composition)
- Reducing body fat (which we know does increase testosterone)
- Improving insulin sensitivity
- Enhancing mood and energy
- Reducing all-cause mortality
Exercise is essential. Just don't promise clients their testosterone will shoot up from lifting weights. The evidence doesn't support that claim.
How to talk about this with clients: Frame strength training honestly. "Strength training builds muscle, helps with body composition, and supports overall metabolic health. Those things indirectly support healthy testosterone. But I want to be honest. Research doesn't show that lifting weights directly raises resting testosterone levels in most men."
Stress Management: The Cortisol Connection¶
Cortisol (the "stress hormone") and testosterone have an inverse relationship. When cortisol goes up, testosterone tends to go down.
Research on police officers and other high-stress populations shows that acute stress elevates cortisol and suppresses testosterone. The testosterone-to-cortisol ratio declines under stress.
This makes biological sense. When you're in survival mode, reproduction is not a priority. Chronic stress keeps the body in that suppressed state.
What this means for your client: Stress management isn't just about feeling better. It may support hormonal health. The interventions here overlap with what you're already coaching: adequate sleep, regular exercise, time in nature, social connection, and explicit stress-reduction practices like meditation or breathwork.
Nutrition: What the Evidence Actually Shows¶
Diet affects testosterone, but not in the ways many people think.
What the research shows:
-
Very low-fat diets lower testosterone. A meta-analysis found that low-fat diet interventions produced modest but significant reductions in serum testosterone compared with higher-fat diets. Men need adequate dietary fat for hormone production.
-
Very high-protein diets (above 3.4 g/kg/day) lower testosterone. This is an extreme intake: for a 180-pound man, that's over 275 grams of protein daily. Normal high-protein intakes (1.2-2.0 g/kg) do not show this effect.
-
Mediterranean-style diets may support healthy testosterone. A small randomized trial found that a low-carbohydrate, Mediterranean-style diet increased serum testosterone.
Coaching takeaway: No single food or supplement "balances hormones" (despite what you'll see on social media). The evidence points to overall dietary patterns: adequate but not excessive protein, sufficient healthy fats, plenty of vegetables, and avoiding extreme restrictions. This is standard good nutrition. Nothing magical required. (No "testosterone superfood" shopping list needed.)
What Lifestyle Can and Cannot Achieve¶
Let's be realistic about expectations.
Lifestyle strategies CAN:
- Support healthy testosterone in men whose levels are being suppressed by modifiable factors (obesity, poor sleep, chronic stress)
- Improve overall health, energy, and body composition, which matters regardless of testosterone numbers
- Prevent further decline by maintaining healthy habits
Lifestyle strategies CANNOT:
- "Cure" genuine hypogonadism caused by testicular or pituitary disease
- Raise testosterone to supraphysiologic levels
- Substitute for medical treatment in men who truly need it
What this means for your client: Be honest. "Lifestyle changes can make a real difference, especially if there are modifiable factors contributing to your symptoms. But if there's an underlying medical condition, lifestyle alone may not be enough. That's where working with your doctor becomes important." Being upfront about these limits actually builds trust.
Coaching in practice: Building a lifestyle game plan for testosterone support¶
The scenario: Your client is worried about testosterone and wants to know what to do.
What NOT to do: Jump straight to lab numbers or supplements without understanding what daily life looks like. That skips over the biggest levers you can actually help with.
What TO do instead: Start with a clear picture of your client's sleep, movement, stress, and nutrition, then pick one or two big wins.
Sample dialogue (first-session focus):
Coach: "Since you're worried about testosterone, can I ask a few questions about sleep, movement, stress, and nutrition? Those are the areas we know make the biggest difference."
Client: "Sure."
Coach: "How many hours of sleep do you usually get? How's your stress level these days?"
Client: "Honestly, I sleep about 5 hours and I'm stressed most of the time."
Coach: "Thanks for sharing that. Based on what you've told me, it sounds like sleep and late-night snacking are the biggest opportunities. How would you feel about focusing on those first?"
Practical checklist you can use:
- Get a clear picture of their lifestyle:
- Sleep: How many hours? How consistent? Quality indicators?
- Body composition: What's the waist circumference? Trend over time?
- Exercise: Strength training frequency? Types of movement?
- Stress: Chronic stressors? Recovery practices?
- Nutrition: Overall pattern? Protein adequacy? Fat intake? Alcohol?
- Prioritize based on biggest gaps:
- Overweight client sleeping 5 hours → Sleep and body composition are priorities
- Lean client with high stress → Stress management and sleep
- Set realistic expectations:
"These changes support overall health and may help with the symptoms you're experiencing. If we make progress on these and you're still concerned, or if symptoms are significant, that's when getting proper testing from your doctor makes sense." - Track progress on what matters:
Energy, mood, sleep quality, body composition, strength, not testosterone numbers (which you can't interpret anyway).
[CHONK: TRT: What Coaches Should Know (Educational)]
Testosterone Replacement Therapy: What Coaches Should Know¶
Now let's cover testosterone replacement therapy (TRT), not so you can advise on it, but so you can be knowledgeable when clients bring it up.
Critical reminder: Everything in this section is educational. Coaches do not recommend for or against TRT. This is a medical decision between a patient and their physician.
When TRT Is Medically Appropriate¶
According to major medical guidelines (Endocrine Society, American Urological Association), testosterone therapy is indicated for men with:
- Consistent symptoms of androgen deficiency
- Unequivocally low testosterone confirmed on at least two morning tests
- After appropriate workup to identify underlying causes
Treatment is NOT recommended for:
- Asymptomatic men with low testosterone numbers
- Men with borderline-low testosterone who haven't had confirmation testing
- Men with reversible causes of low testosterone (like obesity) that should be addressed first
How TRT Works¶
Testosterone replacement provides exogenous (from outside the body) testosterone to restore levels to the normal range. It comes in several forms:
- Injections (intramuscular or subcutaneous): Most common. Can be done at home. Levels fluctuate between injections.
- Transdermal gels or patches: Applied daily. More stable levels but risk of transfer to partners/children.
- Pellets: Implanted under the skin every 3-6 months. Consistent levels but require a procedure.
- Oral formulations: Newer options that avoid liver issues of older oral testosterone. Less commonly used.
The goal is to achieve testosterone levels in the mid-normal range, not supraphysiologic peaks.
What the Evidence Shows About Benefits¶
Recent high-quality evidence has clarified what TRT can and cannot do:
Sexual function: The TRAVERSE trial (the largest cardiovascular safety trial of TRT) found that testosterone improved sexual activity (about 0.47 more acts per day compared to placebo) and sexual desire. However, erectile function did not significantly improve compared to placebo in this study. Translation: TRT may help with desire and activity, but it's not necessarily a fix for erectile dysfunction.
Energy and vitality: Benefits here are more modest and inconsistent. The Endocrine Society Scientific Statement notes "minimal benefits in vitality/strength" from trials in older men.
Body composition: Some improvement in lean mass and reduction in fat mass, though effects are modest.
Bone density: Improvements observed, particularly relevant for men with osteoporosis.
Mood: Some improvement in mood and depressive symptoms in hypogonadal men.
If it feels hard to keep all of those domains straight, that's OK. The simple takeaway is that TRT can help with specific symptoms in men who truly have low testosterone, but it isn't a cure-all.
Cardiovascular Safety: The Current Evidence¶
This has been a major question, and the evidence has evolved:
The TRAVERSE trial (published in New England Journal of Medicine, 2023) enrolled about 5,200 men aged 45-80 with low testosterone and existing cardiovascular risk factors or cardiovascular disease. Over about 2 years:
- Primary endpoint (cardiovascular death, nonfatal heart attack, nonfatal stroke): 7.0% in TRT group vs. 7.3% in placebo group. No significant difference. The trial demonstrated non-inferiority for cardiovascular safety.
Meta-analyses of 26-35 randomized trials consistently show no increase in major cardiovascular events, heart attacks, strokes, or mortality with TRT in hypogonadal men.
However: The TRAVERSE trial did find higher incidences of atrial fibrillation, acute kidney injury, and pulmonary embolism in the testosterone group. These signals warrant monitoring.
Bottom line: For men with genuine hypogonadism who are appropriately monitored, current evidence does not show increased major cardiovascular events. But it's not risk-free. Monitoring matters.
If that level of detail feels overwhelming, you're not alone. Even physicians debate these studies. You don't need to weigh in on the specifics; you just need to know that appropriate medical monitoring is essential.
Bottom line for coaching: Encourage clients to work with qualified prescribers, keep up with their monitoring, and focus your sessions on the lifestyle habits that support cardiovascular health.
Side Effects and Monitoring Requirements¶
TRT requires ongoing medical supervision. Here's what physicians monitor:
Erythrocytosis (elevated red blood cells): This is the most common side effect. Testosterone stimulates red blood cell production, which can thicken the blood and potentially increase clotting risk.
- Guidelines recommend checking hematocrit at baseline, 3 months, and at least annually
- If hematocrit exceeds about 52-54%, dose adjustment or therapeutic phlebotomy (blood removal) may be needed
- One study found that about 40% of therapeutic phlebotomies at a blood center were for men on testosterone therapy
Prostate monitoring: Current evidence does not show increased prostate cancer incidence in men on monitored TRT. However:
- TRT is contraindicated in men with active, untreated prostate cancer
- PSA and digital rectal exam are monitored at baseline, 3 months, and annually
- Rising PSA warrants urology referral
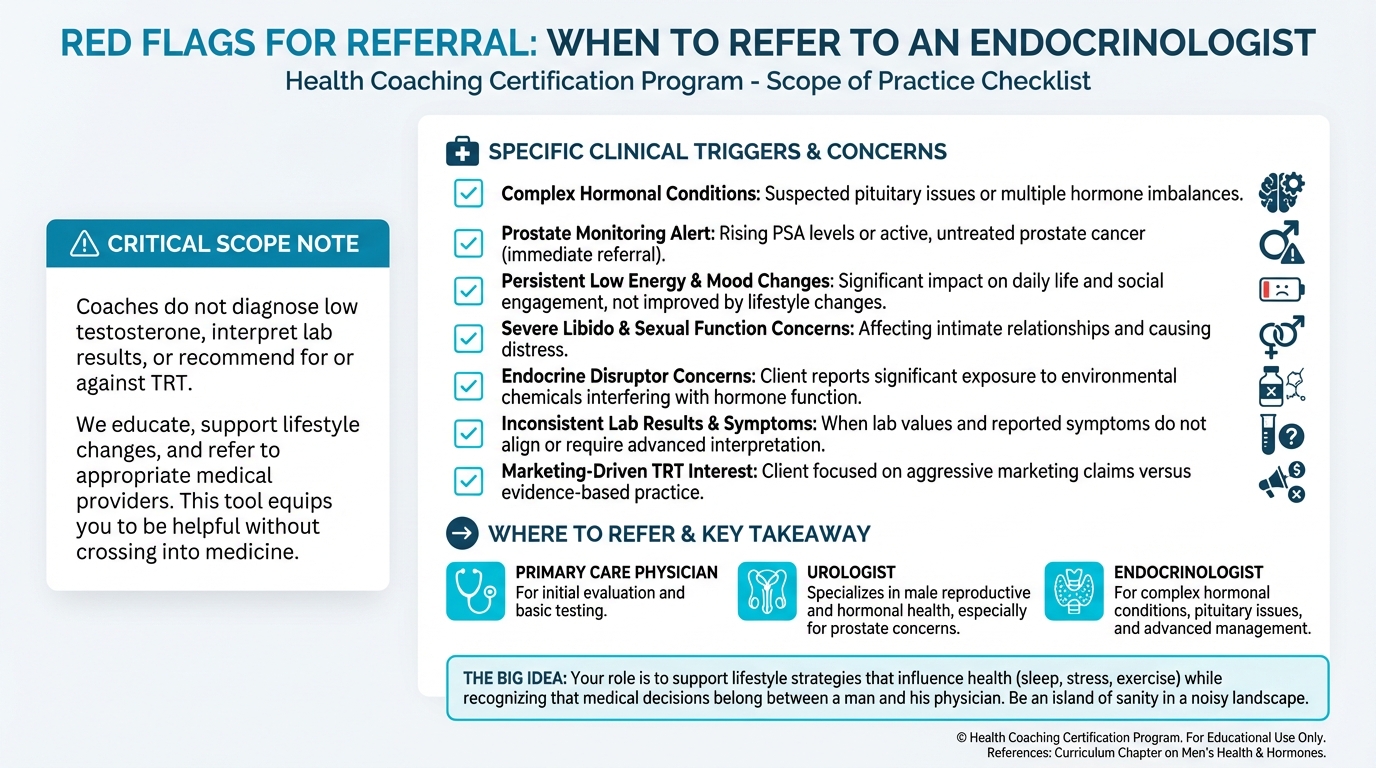
Figure: When to refer to endocrinologist
Other potential side effects:
- Acne and oily skin
- Sleep apnea (can worsen existing sleep apnea)
- Breast enlargement (gynecomastia) if testosterone converts to estrogen
- Mood changes
- Testicular shrinkage (because the body reduces its own production)
CRITICAL: Fertility Implications¶
This section matters enormously, and it's often minimized or ignored in TRT discussions. Exogenous testosterone suppresses sperm production.
Here's the mechanism: When you give testosterone from outside the body, the brain senses "there's enough testosterone" and stops sending signals (LH and FSH) to the testicles to produce more. Without that signal, the testicles not only stop making testosterone, they also stop making sperm.
The statistics are striking:
- Intratesticular testosterone (the testosterone inside the testicles, which is required for sperm production) must fall by more than 80% before spermatogenesis declines. Exogenous testosterone causes exactly this.
- Most men develop severe oligozoospermia (very low sperm count) or azoospermia (zero sperm) within 3-6 months of starting TRT.
- Azoospermia rates reach 90% or higher in controlled male contraceptive trials using testosterone.
- Testicular volume typically decreases by 16-30% during TRT.
Can fertility recover after stopping TRT?
In men who used testosterone for contraceptive studies (typically healthy men with normal baseline fertility):
- About 67% recover to fertile sperm counts by 6 months after stopping
- About 90-98% recover by 12 months
- Nearly 100% recover by 24 months
But: Recovery is slower and often incomplete in men who used TRT long-term (years) or who used anabolic-androgenic steroids at higher doses. In one study of men with prior anabolic steroid use presenting to an infertility clinic, 51% were azoospermic at presentation. Even with treatment (clomiphene + hCG), only 5.6% of initially azoospermic men achieved normal sperm counts at 6 months.
What about preserving fertility while on TRT?
Human chorionic gonadotropin (hCG) mimics the signal (LH) that tells the testicles to produce testosterone. When used alongside TRT, it can maintain intratesticular testosterone and preserve spermatogenesis. Current guidelines recommend gonadotropin therapy (hCG with or without FSH) rather than exogenous testosterone for hypogonadal men who desire future fertility.
What this means for coaching: Any man considering TRT who might want children in the future needs to understand these implications before starting. This isn't optional information. It's essential.
If reading this section feels heavy, that's understandable. The stakes can be high for clients. It's okay if you're still wrapping your head around it; you'll see these ideas again as you revisit the material.
Bottom line for coaching: Make sure clients know that TRT can significantly suppress sperm production, and encourage anyone who might want children in the future to discuss fertility-preserving options with their doctor before starting or changing therapy. Your role is to raise the question, not to predict their fertility or recommend specific protocols.
If a client mentions TRT and is in their reproductive years, asking "Have you discussed the fertility implications with your doctor?" is appropriate and helpful.
Coaching in practice: Explaining fertility implications to clients considering TRT¶
The scenario: A client is considering TRT and may want children in the future.
What NOT to do: Skip over fertility or say, "You can always come off later and you'll be fine."
Why it doesn't work: That minimizes real risks and goes beyond your scope.
What TO do instead: Ask whether future fertility matters to them, share high-level education, and point them back to their doctor for specifics.
Sample dialogue:
Coach: "You mentioned your clinic suggested TRT. Can I ask: Do you have kids already, or is having (more) children something that might matter to you in the future?"
Client: "We might want another child in a few years, but I'm not sure."
Coach: "Thanks for sharing that. One important piece that sometimes gets glossed over is that testosterone replacement can significantly suppress sperm production, often to very low or even zero levels while you're on it. For many men this is reversible after stopping, but it can take many months, and recovery isn't guaranteed, especially with long-term use."
Coach: "If fertility is on your radar at all, it's really important to talk this through with your doctor before starting. There are medical approaches that can help preserve fertility, but they need to be planned in advance."
Scope reminder: Don't advise them whether to start or stop TRT, interpret whether their fertility risk is high or low, or recommend specific protocols. That's their doctor's role.
[CHONK: The TRT Culture Problem]
Navigating the TRT World: Evidence vs. Marketing¶
Your clients are exposed to a massive amount of information about testosterone. Much of it is misleading. As a coach, understanding this environment helps you be a credible, grounded voice amid the noise.
If this whole topic feels confusing or a bit hype-filled, you're in good company. Most clients feel the same way when they first start looking into TRT.
TRT Clinics vs. Evidence-Based Medicine¶
Not all TRT is created equal. There's a meaningful difference between:
Evidence-based TRT (through endocrinologists, urologists, or primary care physicians following guidelines):
- Diagnosis requires confirmed symptoms AND confirmed low testosterone on repeat morning tests
- Treatment targets mid-normal testosterone levels
- Regular monitoring of hematocrit, PSA, symptoms
- Discussion of fertility implications
- Appropriate patient selection
Marketing-driven TRT (some, not all, specialty clinics):
- May diagnose based on symptoms alone or single tests
- May use lower thresholds than major guidelines
- May target testosterone levels above normal range
- May minimize or omit discussion of risks and fertility implications
- May market heavily with promises of life transformation
This isn't to say all TRT clinics are problematic. Many provide excellent care. But the variation in standards is real, and your clients may be navigating it.
The "More Is Better" Myth¶
One dangerous idea circulating in fitness culture is that if normal testosterone is good, higher must be better. This leads to:
Supraphysiologic dosing: Using testosterone doses that push levels well above the normal range.
Here's what the evidence shows about supraphysiologic testosterone:
Cardiovascular effects: While TRT at physiologic doses appears cardiovascular-neutral, animal studies show that supraphysiologic testosterone induces vascular dysfunction through oxidative stress and inflammation pathways. In humans, TRT-induced polycythemia (elevated red blood cells) is associated with increased risk of major adverse cardiovascular events and venous thromboembolism (odds ratio approximately 1.35).
Neurobehavioral effects: Research on anabolic-androgenic steroid users (who use supraphysiologic doses) shows impaired recognition of negative facial expressions compared to non-users. More concerning: approximately 30% of anabolic-androgenic steroid users develop dependence.
Greater suppression of the HPG axis: Higher doses mean more profound suppression of the body's natural testosterone production and more complete suppression of sperm production.
The regulatory picture is also clarifying. In 2025, the FDA determined that appropriately indicated TRT does not show increased cardiovascular risk, and removed prior general cardiovascular risk warnings from labels. But they added warnings about blood pressure increases for certain formulations. The message: physiologic replacement with monitoring is one thing; pushing levels beyond normal is another.
Red Flags in TRT Marketing¶
Help your clients be informed consumers. Some red flags:
- Promises of dramatic life transformation. The evidence shows modest benefits in specific domains, not wholesale transformation.
- "Every man over 40 should consider it." No guideline supports this. TRT is for men with confirmed hypogonadism.
- Dismissal of fertility concerns. "Don't worry about that" or failure to discuss fertility implications.
- Targeting "optimal" rather than "normal." Chasing supraphysiologic levels is not evidence-based.
- Downplaying monitoring needs. Legitimate TRT requires ongoing monitoring. Clinics that minimize this are concerning.
- Aggressive upselling of supplements, peptides, or other add-ons.
Being an Island of Sanity¶
Your role isn't to be anti-TRT. Testosterone replacement is a legitimate treatment for men with genuine hypogonadism. Your role is to help clients:
-
Understand what lifestyle can address first. Many symptoms attributed to "low testosterone" improve with sleep, stress management, and body composition changes.
-
Seek proper diagnosis. Symptoms alone aren't enough. Proper testing (morning, repeated) through appropriate medical providers matters.
-
Ask the right questions. "What's my actual testosterone level?" "Have we confirmed this with a repeat test?" "What are the fertility implications?" "What's the monitoring schedule?"
-
Distinguish marketing from medicine. The flashier the promise, the more skeptical they should be.
Coaching in practice: When a client brings in TRT clinic marketing¶
The scenario: A client brings in TRT clinic marketing and asks what you think.
What NOT to do: Roll your eyes or say, "That place is a scam, stay away." That can shut down the conversation and put you in the role of adversary instead of ally.
What TO do instead: Validate their concerns, then help them think through good questions to ask.
Sample dialogue:
Client: "I saw this clinic that says they can 'optimize my hormones' and get me back to how I felt at 25. What do you think?"
Coach: "I can see why that caught your attention—lots of men are wondering about the same things. Some clinics do great work; others make bigger promises than the evidence supports. Would it be okay if we looked at a few questions you could ask them or your doctor?"
Share evaluation questions: "Some good questions to ask: How do they diagnose low testosterone? Is it based on symptoms alone or confirmed with morning lab tests? What levels are they targeting: mid-normal or higher? What's their monitoring protocol? How do they handle fertility considerations?"
Mention alternatives: "You could also talk to your primary care doctor, a urologist, or an endocrinologist. They follow established guidelines and can provide a second perspective."
Reinforce your role: "My job is to help you with the lifestyle factors that support your health: sleep, exercise, stress, nutrition. Those things matter regardless of what you decide about TRT. And they're often the first things worth addressing before jumping to medical interventions."
[CHONK: Coaching Men Through Hormonal Concerns]
Coaching Men Through Hormone-Related Concerns¶
Let's get practical about your coaching role. This section outlines exactly what you can do, what you cannot do, and how to handle common scenarios.
It’s common to feel a little nervous about saying the "wrong" thing with hormones. That's OK. Caring about scope is part of being a professional.
What Coaches CAN Do¶
Educate about testosterone and aging. You can share the information in this chapter about what testosterone does, how it changes with age, and what symptoms may indicate low testosterone. Education helps clients understand their situation and ask better questions of their physicians.
Support lifestyle strategies that influence hormone health. This is your core domain. Sleep, body composition, stress management, exercise, nutrition. These all matter for testosterone and for overall health. You can assess where clients stand, help them prioritize, and support behavior change.
Explain what research shows about TRT (without recommending). "Research shows that TRT can improve sexual desire and activity in men with confirmed low testosterone, but it doesn't necessarily fix erectile dysfunction. It also has side effects that require monitoring, especially effects on blood count and fertility." This is education, not recommendation.
Discuss fertility implications. Sharing what exogenous testosterone does to sperm production is educational and important. Encouraging clients to discuss this with their doctor before starting TRT is appropriate.
Encourage appropriate medical evaluation. If a client has symptoms that concern them, suggesting they discuss it with a doctor is helpful and within scope. "That sounds like something worth getting checked out" is fine. "You should get your testosterone tested" starts to cross the line.
Support clients who are already on TRT (without advising on it). If a client is on TRT, you can support their lifestyle, helping them with nutrition, exercise, sleep, stress management. You can ask how they're feeling, whether they're keeping up with monitoring appointments. What you cannot do is comment on whether their dose is appropriate, whether they should continue, or interpret their lab results.
What Coaches CANNOT Do¶
Some of these might feel obvious. Others less so, and that's normal as you're learning.
Recommend for or against TRT. "I think you should consider TRT" or "I don't think you need TRT" are both outside scope. The decision is medical.
Interpret testosterone test results. "Your testosterone is low" or "That number is fine" are medical interpretations, even if they seem straightforward.
Suggest specific TRT formulations or doses. "Injections are better than gels" or "You should ask about hCG" crosses into medical territory.
Advise on starting, stopping, or adjusting TRT. "Maybe you should try a lower dose" or "Have you thought about coming off it?" are medical decisions.
Diagnose low testosterone or hypogonadism. Even if a client shows you labs, you cannot diagnose. You can acknowledge symptoms and recommend medical evaluation.
Provide opinions on "ideal" testosterone levels. "600 is where you want to be" is not something you're qualified to say.
Scope-Safe Language Patterns¶
Language matters. Here are patterns that keep you in scope:
INSTEAD OF: "You should get your testosterone tested."
SAY: "If you're experiencing those symptoms, it might be worth bringing up with your doctor."
INSTEAD OF: "That testosterone level is low."
SAY: "I can see why you're concerned. Your doctor can help you understand what your numbers mean and whether treatment is indicated."
INSTEAD OF: "TRT would probably help you."
SAY: "Some men with confirmed low testosterone see benefits from treatment. That's something to explore with your physician if testing shows that's what's going on."
INSTEAD OF: "I don't think you need TRT."
SAY: "There are lifestyle factors that can influence testosterone and energy. Would you like to work on those first and see how you feel? If symptoms persist, you can always revisit testing with your doctor."
INSTEAD OF: "Your TRT dose seems high."
SAY: "How are you feeling on your current regimen? Are you staying on top of your monitoring appointments?"
When to Refer: Specific Criteria¶
Referral to appropriate medical providers is part of your role. Here are clear triggers:
Refer when a client:
- Has symptoms suggestive of low testosterone (reduced libido, fatigue, mood changes, decreased muscle/strength, erectile dysfunction) that haven't been medically evaluated
- Asks about TRT or wants to pursue it
- Has lab results they want interpreted
- Shows signs of potential pituitary issues (severe headaches, visual changes, multiple hormone abnormalities)
- Has fertility concerns alongside testosterone concerns
- Is requesting supplement recommendations for testosterone support
- Has symptoms that aren't improving despite lifestyle changes
Where to refer:
- Primary care physician (for initial evaluation and basic testing)
- Urologist (specializes in male reproductive and hormonal health)
- Endocrinologist (for complex hormonal conditions, pituitary issues)
Working with Medical Teams: Triangle of Care¶
Remember the Triangle of Care model from Chapter 1.5: Client, Coach, Physician working together.
Your role is complementary to medical care, not a replacement for it. For men with confirmed hypogonadism on TRT, you can:
- Support adherence to their treatment plan
- Help with lifestyle factors that complement treatment
- Encourage them to maintain monitoring appointments
- Notice if they're having difficulties they should bring up with their doctor
What you cannot do is make adjustments to the medical side of their care.
Coaching in practice: Scope-safe responses to common testosterone questions¶
The scenario: Clients ask direct questions about testosterone, TRT, or lab results.
What NOT to do (general pattern): Give direct medical advice, interpret lab results, or reassure/dismiss in ways that a physician should.
What TO do instead: Acknowledge the question, stay in your lane, and use language that points back to their medical team while keeping coaching momentum.
When a client asks, "What testosterone level should I aim for?"
You might say: "That's really a question for your doctor. Guidelines target mid-normal ranges, but what's appropriate for you specifically depends on your symptoms, your health history, and your individual response."
When a client asks, "What supplements boost testosterone?"
You might say: "I'm not able to recommend supplements. That's outside my scope as a coach. What I can tell you is that the evidence for most 'testosterone-boosting' supplements is pretty weak. The lifestyle factors that have the most evidence—sleep, body composition, stress management, strength training—are things we can absolutely work on together."
When a client asks, "Should I start TRT?"
You might say: "That's a medical decision I'm not qualified to make. What I can say is that if you're experiencing symptoms, getting properly evaluated is worthwhile. And regardless of what you decide about TRT, the lifestyle factors we work on matter for your health."
When a client says, "My testosterone came back at 350. Is that low?"
You might say: "I can't interpret lab results for you, but that's definitely a question for your doctor. They can tell you what your number means in context of your symptoms, your age, and whether repeat testing is indicated."
[CHONK: Deep Health Integration]
Testosterone and Deep Health: The Bigger Picture¶
Testosterone doesn't exist in isolation. Like everything we address in coaching, it connects to all six dimensions of Deep Health.
Physical¶
Testosterone influences muscle mass, bone density, fat distribution, energy, and sexual function. But the relationship goes both ways. Physical health practices (exercise, sleep, nutrition) also influence testosterone. This is where your coaching has the most direct impact.
Emotional¶
Testosterone affects mood. Men with genuinely low testosterone often report depressive symptoms, irritability, and emotional flatness. But here's the complexity: depression, stress, and anxiety can also suppress testosterone. Addressing emotional health through coaching may have hormonal benefits, and addressing hormonal health may have emotional benefits.
Be aware that for some men, testosterone concerns are wrapped up in feelings about aging, masculinity, and self-worth. If that feels like big territory to hold as a coach, that's understandable. Sensitivity matters here. The goal isn't to dismiss these feelings. It's to support the whole person while staying in scope.
Mental/Cognitive¶
Some men with low testosterone report cognitive symptoms: "brain fog," difficulty concentrating, memory issues. The evidence connecting testosterone to cognition is complex and not fully settled. What we do know: the lifestyle factors that support testosterone (sleep, exercise, stress management) also support cognitive function through multiple pathways.
Social¶
Testosterone influences libido and sexual function, which affect intimate relationships. Low energy and mood changes affect social engagement more broadly. When supporting men with testosterone concerns, be aware of the relational context. Sometimes the distress isn't just about numbers. It's about how they feel in their relationships.
Environmental¶
Endocrine disruptors, chemicals that interfere with hormone function, are present in many consumer products. While the degree to which they affect testosterone in real-world exposures is debated, minimizing exposure to things like BPA, phthalates, and certain pesticides is reasonable. This connects to the environmental health work covered elsewhere in the curriculum.
Existential¶
For many men, concerns about testosterone are really concerns about aging. "Am I still the man I was?" "Am I declining?" "Will I be able to do the things that matter to me?"
This is existential territory. Your role isn't to promise that addressing testosterone will solve these concerns. Your role is to support clients in living well, maintaining the health, strength, and vitality to pursue what matters to them. That's true regardless of their testosterone numbers. You don't need perfect words for every fear; simply listening and staying curious goes a long way. (Really.)
[CHONK: Study guide questions]
Study Guide Questions¶
Here are some questions that can help you think through the material and prepare for the chapter exam. They're optional, but we recommend you try answering at least a few as part of your active learning process.
-
What's the difference between "andropause" and menopause, and why does this distinction matter for how you educate clients?
-
A client asks you to look at their testosterone lab results and tell them if they're "low." What do you say, and why?
-
Of the lifestyle factors that influence testosterone, which has the strongest evidence, and what's a realistic expectation for its effect?
-
What does exogenous testosterone do to sperm production, and why is this important information for clients to know before starting TRT?
-
How would you distinguish between evidence-based TRT practice and marketing-driven practice? What are some "red flags" in TRT marketing?
-
Give an example of scope-safe language for each of these situations:
- A client wants to know if their testosterone is "good"
- A client asks if they should start TRT
-
A client asks what supplements boost testosterone
-
When should you refer a client to a medical provider for testosterone-related concerns? List at least three specific situations.
-
What is polycythemia (erythrocytosis), and why is it monitored in men on TRT?
Self-reflection questions:
-
If you're a man: Before considering any testosterone intervention, how solid are your fundamentals? Sleep, stress management, exercise, body composition—these matter more than any supplement.
-
How has marketing shaped your beliefs about testosterone and aging? Where might you have absorbed messages that aren't supported by evidence?
Chapter Exam¶
Question 1: Testosterone levels in men typically begin declining around what age?
A) 20-25
B) 30-40
C) 50-55
D) 60-65
Question 2: Which of the following is required for a medical diagnosis of hypogonadism according to major guidelines?
A) Symptoms of low testosterone alone
B) A single low testosterone test
C) Consistent symptoms AND low testosterone confirmed on at least two morning tests
D) Age over 40 plus any symptoms
Question 3: Of the following lifestyle factors, which has the strongest evidence for increasing testosterone?
A) High-intensity resistance training
B) Meditation and stress reduction
C) Weight loss in overweight men
D) Sleep extension from 7 to 9 hours
Question 4: True or False: Research consistently shows that chronic resistance training significantly increases resting testosterone levels in healthy adult men.
A) True
B) False
Question 5: What happens to sperm production when a man takes exogenous testosterone?
A) It typically increases
B) It remains unchanged
C) It is typically suppressed significantly, often to near-zero levels
D) It fluctuates unpredictably
Question 6: According to the TRAVERSE trial, what was the finding regarding major cardiovascular events (heart attack, stroke, cardiovascular death) in men on TRT versus placebo?
A) TRT significantly increased cardiovascular events
B) TRT significantly decreased cardiovascular events
C) There was no significant difference between groups
D) The trial was stopped early due to safety concerns
Question 7: Polycythemia (elevated red blood cells) during TRT is associated with:
A) Improved oxygen delivery and athletic performance
B) Increased risk of clotting and potentially cardiovascular events
C) No clinical significance
D) Improved testosterone response
Question 8: A client asks you to tell them whether their testosterone level of 310 ng/dL is "low." The scope-appropriate response is:
A) "That's borderline low. You might want to consider TRT."
B) "That's actually fine. You don't need to worry."
C) "I can't interpret lab results for you, but your doctor can help you understand what your numbers mean in your specific context."
D) "Let me look up the reference ranges and tell you where you fall."
Question 9: Which of the following is within a health coach's scope of practice?
A) Recommending that a client start TRT
B) Interpreting testosterone lab results
C) Supporting lifestyle changes that may influence testosterone
D) Advising on TRT dosing
Question 10: What is hCG (human chorionic gonadotropin), and why might it be used in the context of TRT?
A) A supplement that boosts natural testosterone production
B) A hormone that mimics LH and can help preserve fertility in men on TRT
C) A testosterone formulation with fewer side effects
D) A marker used to diagnose low testosterone
Question 11: True or False: "Andropause" in men is biologically equivalent to menopause in women, involving an abrupt and universal cessation of hormone production.
A) True
B) False
Question 12: A "red flag" in TRT clinic marketing would be:
A) Requiring two morning testosterone tests before diagnosis
B) Discussing fertility implications of treatment
C) Promising dramatic life transformation and targeting "optimal" rather than normal testosterone levels
D) Having a structured monitoring protocol
Question 13: After stopping TRT, approximately what percentage of men (in controlled contraceptive studies) recover to fertile sperm counts by 12 months?
A) 25-35%
B) 50-60%
C) 90-98%
D) 100% always
Question 14: Which of the following dietary patterns has evidence suggesting it may support healthy testosterone?
A) Very low-fat diet
B) Very high-protein diet (>3.4 g/kg/day)
C) Mediterranean-style diet with adequate healthy fats
D) Strict ketogenic diet with protein restriction
Question 15: When a client expresses concern about testosterone and hasn't seen a doctor, the most appropriate coach response is:
A) "Let's get your testosterone tested. I can help you interpret the results."
B) "You're probably fine, don't worry about it."
C) "I'd suggest discussing this with your doctor. In the meantime, we can work on lifestyle factors that support overall health and may influence these symptoms."
D) "Based on your symptoms, you almost certainly have low testosterone."
Works cited¶
References¶
-
Abdel-Sater KA. The role of anti-aging approaches in managing hypogonadism in sedentary older males. Frontiers in Aging. 2024;5. doi:10.3389/fragi.2024.1514438
-
Santi D, Spaggiari G, Furini C, Griseta V, Zizzi E, Raffaele MGA, et al. Temporal trends in serum testosterone and luteinizing hormone levels indicate an ongoing resetting of hypothalamic-pituitary-gonadal function in healthy men: a systematic review. Endocrine Abstracts. 2025. doi:10.1530/endoabs.110.ep1326
-
Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, Matsumoto AM, et al. Testosterone Therapy in Men With Hypogonadism: An Endocrine Society* Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism. 2018;103(5):1715-1744. doi:10.1210/jc.2018-00229
-
Mulhall JP, Trost LW, Brannigan RE, Kurtz EG, Redmon JB, Chiles KA, et al. Evaluation and Management of Testosterone Deficiency: AUA Guideline. Journal of Urology. 2018;200(2):423-432. doi:10.1016/j.juro.2018.03.115
-
Cappola AR, Auchus RJ, El-Hajj Fuleihan G, Handelsman DJ, Kalyani RR, McClung M, et al. Hormones and Aging: An Endocrine Society Scientific Statement. The Journal of Clinical Endocrinology & Metabolism. 2023;108(8):1835-1874. doi:10.1210/clinem/dgad225
-
Travison TG, Vesper HW, Orwoll E, Wu F, Kaufman JM, Wang Y, et al. Harmonized Reference Ranges for Circulating Testosterone Levels in Men of Four Cohort Studies in the United States and Europe. The Journal of Clinical Endocrinology & Metabolism. 2017;102(4):1161-1173. doi:10.1210/jc.2016-2935
-
Su L, Zhang S, Zhu J, Wu J, Jiao Y. Effect of partial and total sleep deprivation on serum testosterone in healthy males: a systematic review and meta-analysis. Sleep Medicine. 2021;88:267-273. doi:10.1016/j.sleep.2021.10.031
-
Hernández‐Pérez JG, Taha S, Torres‐Sánchez LE, Villasante‐Tezanos A, Milani SA, Baillargeon J, et al. Association of sleep duration and quality with serum testosterone concentrations among men and women: NHANES 2011–2016. Andrology. 2023;12(3):518-526. doi:10.1111/andr.13496
-
Potter NJ, Tomkinson GR, Dufner TJ, Walch TJ, Roemmich JN, Wilson PB, et al. Effects of Exercise Training on Resting Testosterone Concentrations in Insufficiently Active Men: A Systematic Review and Meta-Analysis. Journal of Strength & Conditioning Research. 2021;35(12):3521-3528. doi:10.1519/jsc.0000000000004146
-
Hayes LD, Elliott BT. Short-Term Exercise Training Inconsistently Influences Basal Testosterone in Older Men: A Systematic Review and Meta-Analysis. Frontiers in Physiology. 2019;9. doi:10.3389/fphys.2018.01878
-
Ikehata Y, Hachiya T, Kobayashi T, Ide H, Horie S. Body composition and testosterone in men: a Mendelian randomization study. Frontiers in Endocrinology. 2023;14. doi:10.3389/fendo.2023.1277393
-
Okobi OE, Khoury P, De la Vega RJ, Figueroa RS, Desai D, Mangiliman BDA, et al. Impact of Weight Loss on Testosterone Levels: A Review of BMI and Testosterone. Cureus. 2024. doi:10.7759/cureus.76139
-
Whittaker J. High-protein diets and testosterone. Nutrition and Health. 2022;29(2):185-191. doi:10.1177/02601060221132922
-
Whittaker J, Wu K. Low-fat diets and testosterone in men: Systematic review and meta-analysis of intervention studies. The Journal of Steroid Biochemistry and Molecular Biology. 2021;210:105878. doi:10.1016/j.jsbmb.2021.105878
-
Lincoff AM, Bhasin S, Flevaris P, Mitchell LM, Basaria S, Boden WE, et al. Cardiovascular Safety of Testosterone-Replacement Therapy. New England Journal of Medicine. 2023;389(2):107-117. doi:10.1056/nejmoa2215025
-
Pencina KM, Travison TG, Cunningham GR, Lincoff AM, Nissen SE, Khera M, et al. Effect of Testosterone Replacement Therapy on Sexual Function and Hypogonadal Symptoms in Men with Hypogonadism. The Journal of Clinical Endocrinology & Metabolism. 2023;109(2):569-580. doi:10.1210/clinem/dgad484
-
Cruickshank M, Hudson J, Hernández R, Aceves-Martins M, Quinton R, Gillies K, et al. The effects and safety of testosterone replacement therapy for men with hypogonadism: the TestES evidence synthesis and economic evaluation. Health Technology Assessment. 2024:1-210. doi:10.3310/jryt3981
-
Elagizi A, Köhler TS, Lavie CJ. Testosterone and Cardiovascular Health. Mayo Clinic Proceedings. 2018;93(1):83-100. doi:10.1016/j.mayocp.2017.11.006
-
Basheer B, Ila V, Barros R, Mesquita F, Lopes LS, Lima VFN, et al. Management of Adverse Effects in Testosterone Replacement Therapy. International braz j urol. 2025;51(3). doi:10.1590/s1677-5538.ibju.2025.9904
-
Desai A, Yassin M, Cayetano A, Tharakan T, Jayasena CN, Minhas S. Understanding and managing the suppression of spermatogenesis caused by testosterone replacement therapy (TRT) and anabolic–androgenic steroids (AAS). Therapeutic Advances in Urology. 2022;14. doi:10.1177/17562872221105017
-
Hashimi MA, Pinggera G, Shah R, Agarwal A. Clinician’s guide to the management of azoospermia induced by exogenous testosterone or anabolic–androgenic steroids. Asian Journal of Andrology. 2025;27(3):330-341. doi:10.4103/aja2024104
-
Fink J, Ide H, Horie S. Management of Male Fertility in Hypogonadal Patients on Testosterone Replacement Therapy. Medicina. 2024;60(2):275. doi:10.3390/medicina60020275
-
Coward R, McBride J. Recovery of spermatogenesis following testosterone replacement therapy or anabolic-androgenic steroid use. Asian Journal of Andrology. 2016;18(3):373. doi:10.4103/1008-682x.173938
-
Ledesma BR, Weber A, Venigalla G, Muthigi A, Thomas J, Narasimman M, et al. Fertility outcomes in men with prior history of anabolic steroid use. Fertility and Sterility. 2023;120(6):1203-1209. doi:10.1016/j.fertnstert.2023.09.016
-
Scarth M, Hauger LE, Thorsby PM, Leknes S, Hullstein IR, Westlye LT, et al. Supraphysiological testosterone levels from anabolic steroid use and reduced sensitivity to negative facial expressions in men. 2023. doi:10.31234/osf.io/h854w
-
Alves JV, da Costa RM, Pereira CA, Fedoce AG, Silva CAA, Carneiro FS, et al. Supraphysiological Levels of Testosterone Induce Vascular Dysfunction via Activation of the NLRP3 Inflammasome. Frontiers in Immunology. 2020;11. doi:10.3389/fimmu.2020.01647
-
National Board for Health & Wellness Coaching. NBHWC Health & Wellness Coach Scope of Practice. 2023. https://nbhwc.org/scope-of-practice/
-
Gulati M. Lifestyle Medicine’s Role in Common Hormonal Disorders: A Case-Based Discussion. American Journal of Lifestyle Medicine. 2024;18(5):638-647. doi:10.1177/15598276241242012