Unit 3: Advanced Topics & Disease Prevention¶
Chapter 3.20: Supporting Women's Hormonal Health¶
[CHONK: 1-minute summary]
[CHONK: Introduction and Context]
Why this chapter matters¶
At some point, every woman goes through menopause. It's not a disease or a disorder; it's a normal biological transition, and yet it affects nearly every system in the body, from sleep to mood to bone health to cardiovascular risk.
As a coach, you'll work with women who are navigating this transition. Some will breeze through with minimal symptoms. Others will experience changes that significantly affect their daily lives, their training, their relationships, and their sense of self.
This chapter gives you the knowledge to support these clients effectively, and the wisdom to know where your support ends and medical care begins.
What makes this chapter different from others is that hormone replacement therapy (HRT) is a medical decision that sits firmly outside your scope as a coach. You cannot recommend for or against HRT. You cannot interpret hormone labs. You cannot advise on formulations or dosages.
What you can do is understand what's happening physiologically, help clients with lifestyle factors that genuinely matter, and know when to encourage conversations with healthcare providers.
That's what this chapter teaches you to do.
Learning objectives¶
By the end of this chapter, you'll be able to:
- Explain the physiology of perimenopause and menopause, including key hormonal changes and their effects on multiple body systems
- Discuss HRT with appropriate scope: educating about evidence without recommending for or against
- Describe training and nutrition adjustments that support women through hormonal transitions
- Support clients through menopause without overstepping into medical practice
- Identify when hormonal symptoms require referral to appropriate medical specialists
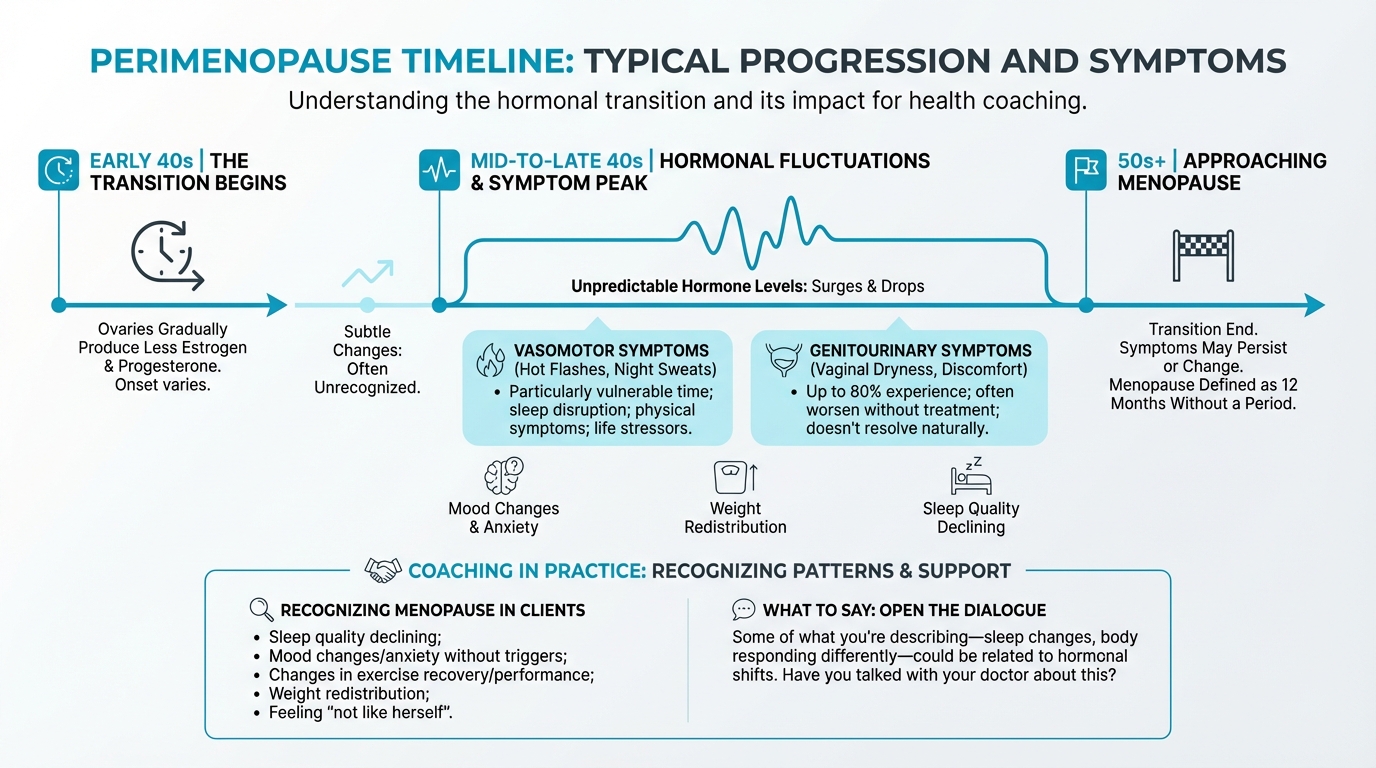
Figure: Typical progression and symptoms
[CHONK: The Menopause Transition]
What happens during menopause¶
Let's start with definitions. These terms get used loosely, so let's be precise.
Perimenopause: The transition begins¶
Perimenopause, also called the menopausal transition, is the time leading up to menopause. It typically begins in a woman's mid-to-late 40s, though it can start earlier.
During perimenopause, the ovaries gradually produce less estrogen and progesterone. But this isn't a smooth, linear decline. Hormone levels fluctuate unpredictably, sometimes surging higher than ever before, then dropping. These fluctuations drive many of the symptoms women experience.
How long does it last?
- The median duration is about four years
- It commonly ranges from two to eight years
- Some women experience transitions lasting 10 to 14 years
- Women who start earlier tend to have longer transitions
The STRAW+10 staging system (Stages of Reproductive Aging Workshop) defines perimenopause as spanning from the onset of menstrual cycle changes through 12 months after the final menstrual period.
Menopause: A specific moment¶
Menopause itself is a single point in time: the moment when a woman has gone 12 consecutive months without a menstrual period (assuming no other cause).
- Average age: 51-52 years
- Typical range: 45-58 years
- Defined retrospectively: you only know it happened after a year without periods
Types of menopause¶
Not all menopause is the same:
Natural menopause occurs when estrogen and progesterone decline naturally with aging.
Surgical menopause happens when the ovaries are removed (oophorectomy). Because hormone levels drop suddenly rather than gradually, symptoms often begin immediately and may be more intense.
Premature menopause (or premature ovarian insufficiency) occurs before age 40. This affects about 1 in 100 women before 40 and 1 in 1,000 before 30. Risk factors include certain medical conditions, treatments like chemotherapy, smoking, and genetic factors.
The hormones involved¶
Several hormones change during this transition:
Estrogen is actually a family of hormones: estrone (E1), estradiol (E2), and estriol (E3). Estradiol is the primary estrogen during reproductive years. After menopause, estrone becomes dominant but at much lower overall levels.
Progesterone drops as ovulation becomes irregular, then ceases entirely after menopause.
Follicle-stimulating hormone (FSH) rises as the brain tries to signal the ovaries to produce more estrogen. High FSH levels can help confirm menopausal status.
Luteinizing hormone (LH) also increases during the transition.
Why these changes affect the whole body¶
Estrogen receptors exist throughout the body, not just in reproductive organs. When estrogen levels drop, systems throughout the body are affected:
- Brain: Mood regulation, cognitive function, temperature control
- Cardiovascular system: Blood vessel function, cholesterol metabolism
- Bones: Bone remodeling and density maintenance
- Skin: Collagen production, moisture retention
- Urogenital tract: Vaginal tissue health, urinary function
- Muscles: Protein synthesis, muscle maintenance
This is why menopause symptoms extend far beyond hot flashes.
Common symptoms and their impact¶
Vasomotor symptoms: Hot flashes and night sweats¶
These are the symptoms most associated with menopause:
- About 57 percent of women aged 40-64 experience vasomotor symptoms
- 15-20 percent experience moderate-to-severe symptoms
- Symptoms can persist for seven or more years after menopause
- Prevalence and severity vary significantly by individual and demographic factors
Hot flashes involve a sudden sensation of heat, often accompanied by flushing and sweating. When they occur at night (night sweats), they can significantly disrupt sleep.
Sleep disruption¶
Sleep problems are extremely common:
- 40-60 percent of menopausal women report significant sleep problems
- About half of postmenopausal women meet criteria for at least one sleep disorder
- About 26 percent experience symptoms consistent with clinical insomnia
- Restless legs syndrome also shows high prevalence
Sleep disruption often connects to night sweats but can occur independently. Some women wake from hot flashes; others simply have difficulty falling asleep or staying asleep even without obvious triggers.
Why sleep disruption matters so much:
Poor sleep compounds every other symptom. It affects:
- Mood regulation and emotional resilience
- Cognitive function (worsening "brain fog")
- Appetite hormones (increasing hunger, particularly for high-calorie foods)
- Recovery from exercise
- Energy and motivation for healthy behaviors
- Immune function
This is why sleep environment and sleep hygiene should be early priorities when coaching menopausal clients. Addressing sleep often creates a positive cascade into other areas.
Mood changes¶
Depression and anxiety occur more frequently during the menopausal transition:
- The perimenopause appears to be a particularly vulnerable time
- Changes relate partly to hormonal fluctuations and partly to life circumstances
- Sleep disruption, physical symptoms, and life stressors all contribute
Cognitive changes¶
Many women report cognitive changes, often called "brain fog":
- 44-62 percent of perimenopausal women report memory problems
- 60-70 percent of midlife women report memory or concentration concerns
- Objective testing shows small but reliable declines in verbal memory and executive function during the transition
- For most women, performance remains within normal limits
Current guidelines do not recommend hormone therapy specifically for cognitive symptoms.
Body composition changes¶
Menopause is associated with shifts in body composition:
- Average weight gain of 2-3 kg during the transition
- Shift toward central and visceral fat accumulation
- Decline in lean muscle mass
- These changes occur partly from hormonal shifts and partly from aging itself
Bone loss¶
The skeletal impact is significant:
- Estrogen helps maintain bone density; its decline accelerates bone loss
- Women can lose 1-5 percent of bone mineral density per year in the first 5-7 years after menopause
- About one in two women over 50 will experience an osteoporotic fracture
- Hip fractures carry 12-20 percent one-year mortality in older women
Genitourinary changes¶
Changes to vaginal and urinary tissue are common but often underdiscussed:
- Up to 80 percent of menopausal women experience genitourinary symptoms
- These include vaginal dryness, discomfort during sex, and urinary symptoms
- Unlike hot flashes, these symptoms typically don't resolve over time. They often worsen without treatment
Cardiovascular changes¶
Menopause accelerates cardiovascular risk:
- Loss of estrogen's protective effects on blood vessels
- Shifts in cholesterol patterns (increased LDL, decreased HDL)
- Increased visceral fat and insulin resistance
- The "cardiovascular gap" between men and women narrows after menopause
Individual variation is enormous¶
Perhaps the most important thing to understand: no two women experience menopause the same way.
Some women have minimal symptoms. Others are significantly affected. Duration, severity, and which symptoms predominate all vary widely. Race, ethnicity, body composition, lifestyle factors, and genetics all influence the experience.
Research shows meaningful differences across populations:
- African-American women tend to have longer menopausal transitions and more severe vasomotor symptoms
- Smoking is associated with earlier menopause onset
- Higher body mass index is associated with later onset
- Geographic and cultural factors influence both symptom reporting and treatment-seeking
This variation means cookie-cutter approaches don't work. What helps one client may not help another. Your role is to understand the individual in front of you—her specific symptoms, her context, her goals—and adapt your support accordingly.
If that feels like a lot to keep track of, you're not alone. You don't need to memorize every pattern; you just need to stay curious about the person in front of you.
Coaching in practice: Recognizing menopause in your clients¶
The scenario: Your client is in her early-to-mid 40s. She's noticing changes in sleep, mood, and how her body responds to training, but she hasn't connected any of this to hormones.
She might say things like, "I'm not sleeping as well," "I feel more anxious for no reason," or "My workouts wipe me out now," without realizing these shifts could be part of the menopausal transition.
Common patterns to notice include:
- Sleep quality declining for no obvious reason
- Mood changes or increased anxiety without clear triggers
- Changes in exercise recovery or performance
- Weight redistribution despite consistent habits
- Reports of feeling "not like herself"
What NOT to do:
❌ Tell her, "Oh, this is definitely perimenopause," or suggest specific medical treatments.
Why it doesn't work: You're stepping into diagnosing and medical decision-making, which is outside your scope.
What TO do:
✅ Get curious about patterns, reflect what you're hearing, and gently suggest a medical conversation—without labeling or diagnosing.
Sample dialogue:
Client: "I'm doing everything the same, but I'm not sleeping, I'm more on edge, and my workouts feel so much harder. I just don't feel like myself."
Coach: "I hear how much this is affecting you, and that 'not like myself' feeling can be really unsettling. You're noticing changes in sleep, mood, and recovery, and those can have lots of possible causes."
Client: "Yeah, I keep wondering if I'm just stressed or if something else is going on."
Coach: "It could be stress, and it could also be related to hormonal shifts that are common for women in their 40s and 50s. I can't tell you exactly what's happening—that's beyond my role—but it does sound worth talking through with your doctor."
Client: "I hadn't even thought about hormones. What should I say to my doctor?"
Coach: "You might share exactly what you told me: the changes in your sleep, mood, recovery, and how long they've been going on. If you’d like, we can jot down a few notes or questions for your appointment. And whatever your doctor finds, we can keep working on your sleep, training, and nutrition together."
[CHONK: HRT - What Coaches Should Know]
Hormone replacement therapy: An educational overview¶
This section exists because your clients will have questions about HRT. They'll see headlines, hear friends' experiences, and wonder what to do. You need to understand the topic well enough to have informed conversations, while always being clear that HRT decisions belong to medical professionals.
A medical decision, not a coaching decision¶
Before we go further, let's be absolutely clear about scope:
Coaches CAN:
- Explain what HRT is in general terms
- Share that research exists and continues to evolve
- Encourage clients to discuss HRT with their healthcare providers
- Support clients who are using HRT (without commenting on whether they should be)
- Support clients who choose not to use HRT
Coaches CANNOT:
- Recommend for or against HRT
- Suggest specific formulations, doses, or delivery methods
- Interpret hormone lab results
- Advise on starting, stopping, or adjusting HRT
- Express opinions about whether a client "should" be on HRT
When a client asks, "Should I take HRT?" The honest answer is: "That's a medical decision between you and your healthcare provider. I can support you either way with lifestyle factors, but I'm not qualified to advise on hormone therapy."
The WHI controversy and how understanding evolved¶
To understand the current state of HRT, you need to know about the Women's Health Initiative (WHI).
In 2002, the WHI, a large randomized trial, was stopped early when researchers found increased risks of breast cancer, heart disease, and stroke in women taking combined estrogen-progestin therapy. Headlines warned that HRT was dangerous. Many women stopped therapy abruptly. Prescribing dropped dramatically.
But the story didn't end there. As researchers analyzed the data more carefully, a more complex picture emerged:
What the reanalysis showed:
- Age and timing matter enormously. Women who started HRT closer to menopause (within about 10 years of menopause or before age 60) showed different patterns than women who started later.
- Formulation matters. Estrogen-only therapy (for women who've had a hysterectomy) showed different risks than combined estrogen-progestin therapy.
- Route matters. Transdermal (patch or gel) estrogen appears to have lower clotting risks than oral estrogen.
- Progestogen type matters. Micronized progesterone may carry lower breast cancer risk than synthetic progestins, though head-to-head randomized trial data are limited.
The "timing hypothesis"¶
One key concept that emerged from WHI reanalysis is the timing hypothesis (sometimes called the "critical window"):
Starting HRT within about 10 years of menopause onset or before age 60 is associated with a more favorable benefit-risk profile than starting later.
Major guidelines now reflect this: the North American Menopause Society, the Endocrine Society, and international cardiology guidelines all acknowledge this timing effect.
But, and this is important, the timing hypothesis doesn't make HRT "safe" or "recommended." It means the risk-benefit calculation differs based on when therapy starts. Individual factors still drive the decision.
What HRT involves (educational overview)¶
HRT typically includes:
Estrogen: Replaces declining estrogen levels. Available as:
- Oral pills
- Transdermal patches
- Topical gels or creams
- Vaginal preparations (for local symptoms only)
Progestogen: Required for women who have a uterus to protect against endometrial cancer. Options include:
- Synthetic progestins
- Micronized (natural) progesterone
Testosterone: Sometimes prescribed for sexual desire concerns. We'll discuss this separately below.
The choice of formulation, route, and dose depends on individual factors: a medical determination, not a coaching one.
Current evidence: What research shows¶
Current evidence suggests the following (with appropriate caveats):
For symptom relief:
- HRT remains the most effective treatment for vasomotor symptoms
- It effectively treats genitourinary symptoms of menopause
- Effects on mood and sleep vary by individual
For bone health:
- HRT prevents early postmenopausal bone loss
- It reduces fracture risk during use
For cardiovascular outcomes:
- The picture is complex and depends heavily on timing
- Early initiation (near menopause) is associated with more favorable cardiovascular signals
- Late initiation increases cardiovascular risks
- HRT is not recommended for primary cardiovascular disease prevention
For breast cancer:
- Risk depends on formulation and duration
- Estrogen-only therapy shows little or no increase in breast cancer risk
- Combined therapy with synthetic progestins increases risk modestly
- Micronized progesterone may carry lower risk than synthetic progestins (observational data)
- Risk appears to decline after discontinuation
For stroke and blood clots:
- HRT increases stroke risk, particularly with oral formulations and older age
- Venous thromboembolism risk is elevated with oral therapy; transdermal routes appear safer
"Bioidentical" hormones: A note¶
You may hear clients ask about "bioidentical" hormones. This term is often used for hormones chemically identical to those the body produces.
Many FDA-approved HRT products are bioidentical: transdermal estradiol patches and micronized progesterone are examples.
The term is also sometimes used for custom-compounded preparations from compounding pharmacies. These preparations:
- Lack the regulatory oversight of FDA-approved products
- May have potency and quality variations
- Have not been shown to be safer or more effective than approved products
- Are not recommended by major guidelines over approved alternatives
The evidence is evolving¶
Honest conversations about HRT are challenging because the evidence continues to evolve. Research on different formulations, routes, and timing is ongoing, and what we understand today may be refined by future studies.
If you're feeling like the ground keeps shifting here, you're not alone. Even clinicians have had to update their understanding over time.
This is exactly why HRT decisions belong with medical professionals who can integrate the latest evidence with individual patient factors.
Coaching in practice: "Should I take HRT?"¶
The scenario: Your client has been reading articles and talking with friends, and now she asks: "Should I take HRT?"
What NOT to do:
❌ Give a yes-or-no answer or share what you would do in her place.
❌ Say things like:
- "You should definitely consider HRT. It's much safer than people used to think."
- "I wouldn't take HRT if I were you."
- "Your hormones seem low, so you probably need HRT."
- "I think you'd really benefit from bioidentical hormones."
Why it doesn't work: You're stepping into medical decision-making and making assumptions about her health history and risks.
What TO do:
✅ Name your scope, validate the question, and redirect to a medical conversation—while staying available to support lifestyle changes.
Sample dialogue:
Client: "I've been reading so much about hormones, and honestly I'm confused. Should I take HRT?"
Coach: "That's a great question, and it's completely understandable to feel confused. There's a lot of information out there."
Client: "Yeah, everyone seems to say something different."
Coach: "HRT is a medical decision that depends on your health history, your symptoms, and your risk factors, so it's not something I can advise on directly. The best place to sort that out is with your doctor or a menopause specialist."
Client: "So you can't tell me if it's safe?"
Coach: "What I can tell you is that the research on HRT has evolved a lot over the years, and it's definitely worth an informed conversation with your healthcare provider. If you'd like, I can help you think through questions to ask at that appointment, and whatever you and your doctor decide, I'm here to support you with the lifestyle pieces that matter either way."
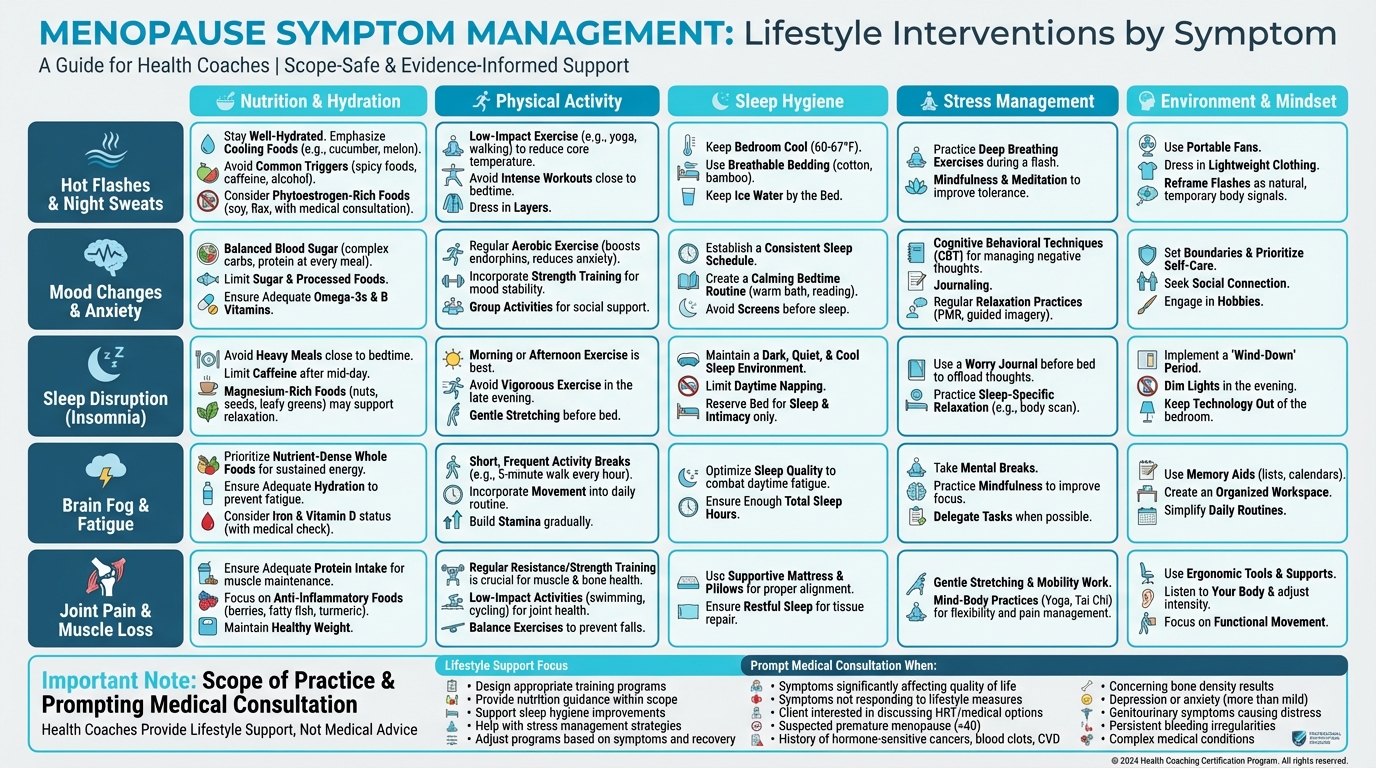
Figure: Lifestyle interventions by symptom
Testosterone for women: Brief note¶
You may hear clients ask about testosterone for women. The key points are:
- Testosterone is sometimes prescribed for hypoactive sexual desire disorder (HSDD) in postmenopausal women
- Clinical trials show modest improvements in sexual desire in selected women
- There is no good evidence that testosterone improves energy, mood, cognition, or general well-being in women
- Long-term safety data are limited
- It is not FDA-approved for use in women in the United States
Current guidelines recommend testosterone only for women with diagnosed HSDD after other causes have been excluded, with careful monitoring and time-limited treatment.
This is firmly a medical decision. Do not recommend testosterone to clients.
Emerging research: A mention¶
You may see headlines about interventions to delay menopause or "preserve ovarian function." Some examples:
mTOR inhibitors (like rapamycin): Early animal studies and a small pilot human trial suggest mTOR inhibitors might slow the activation of follicles in the ovaries. Larger human trials are planned but not complete.
Hyperbaric oxygen therapy (HBOT): Animal studies show some effects on ovarian markers, but no human clinical trials have demonstrated effects on menopause timing.
Big picture: No intervention has been proven in randomized human trials to delay natural menopause. These remain experimental areas of research. They are not ready for clinical application and are not something coaches should discuss as options.
[CHONK: Training Through the Transition]
Exercise for women during hormonal transitions¶
If there's one area where coaches can make a genuine difference for women in menopause, it's exercise. The evidence for exercise benefits during this transition is strong, and this is squarely within coaching scope.
Why strength training matters more during menopause¶
As estrogen declines, women face accelerated losses of both muscle mass and bone density. Strength training directly addresses both.
For muscle preservation:
- Sarcopenia (age-related muscle loss) accelerates after menopause
- Resistance training is the primary intervention to maintain and build muscle
- Postmenopausal women may need higher training volumes than premenopausal women to achieve the same hypertrophy response
- One study found that postmenopausal women needed more than 6-8 sets per muscle group weekly to gain muscle mass, while premenopausal women gained mass at that volume
For bone health:
- Weight-bearing and resistance exercise stimulates bone remodeling
- High-impact activities (jumping, hopping) provide additional bone stimulus
- Meta-analyses show mixed-loading programs (combining impact exercise with resistance training) effectively preserve bone mineral density at the hip and spine
For metabolic health:
- Resistance training helps maintain metabolic rate as muscle mass is preserved
- It improves insulin sensitivity
- Combined with aerobic exercise, it positively affects body composition
What the research shows¶
Research on exercise during menopause shows:
Body composition:
- Resistance training is most effective for maintaining or increasing lean mass
- Aerobic training is most effective for reducing fat mass
- Combined programs deliver the best overall results
Bone mineral density:
- High-impact and high-intensity loading helps preserve bone
- Effects are modest and site-specific
- Combined impact and resistance training appears most effective
- Long-duration studies show clearer benefits than short-term trials
Menopausal symptoms:
- Exercise significantly reduces insomnia severity, particularly in women with baseline sleep problems
- Mood and quality of life generally improve with regular exercise
- Evidence for reducing hot flash frequency is inconsistent. Some women report improvement, but rigorous reviews find no clear effect
One important nuance: During perimenopause itself (while still in transition), short-term exercise studies often show limited changes in bone density and lean mass. Benefits become clearer in early postmenopause with consistent training.
Practical recommendations¶
Resistance training:
- Frequency: 2-4 sessions per week, hitting all major muscle groups across the week
- Exercise selection: Compound movements (squats, deadlifts, rows, presses, lunges) form the foundation. These movements load multiple joints, stimulate more muscle mass, and provide functional carryover to daily life
- Progressive overload is essential: Gradually increase challenge over time: add weight, add reps, add sets. Without progressive challenge, muscles don't adapt
- Volume considerations: Research suggests postmenopausal women may need higher training volumes (more total sets per muscle group) to achieve muscle growth compared to premenopausal women. Don't be afraid to program substantial training
- Intensity matters: Lifting heavy (relative to the individual) provides more stimulus for muscle and bone than high-rep, low-weight approaches. Help clients understand that "heavy" is personal. It's about challenging themselves appropriately
- Recovery: Sleep disruption can impair recovery. You may need to adjust session frequency or intensity during periods of poor sleep
- Focus on strength and function: Frame the goal as getting stronger and more capable, not just "toning." Strength is protective and functional
Impact loading for bones:
- Include jumping, hopping, or skipping if appropriate for the client. These activities provide mechanical loading that stimulates bone remodeling
- Even brief impact sessions provide bone stimulus. This doesn't need to be lengthy
- Progress gradually; consider joint health and fitness level
- For clients with osteoporosis or joint issues, modify or substitute with resistance training
- Examples: jump rope, box step-ups with emphasis on the step-down, low hurdle hops, lateral bounds
- Meta-analyses show mixed-loading programs (combining impact with resistance training) are most effective for preserving bone at the hip and spine
- Start conservatively: 10-20 jumps per session is a reasonable starting point for someone new to impact training
Aerobic training:
- Include for cardiovascular health and fat mass management
- Zone 2 (conversational pace) training 150+ minutes weekly is a solid foundation
- Can be combined with resistance training in the same program
- Consider that cardiovascular risk increases after menopause. Aerobic fitness becomes more important
- Walking is effective and sustainable for many women
- Higher intensities (interval training) may provide additional metabolic benefits but balance with recovery needs
- Swimming and cycling are joint-friendly options for women with joint concerns
Balance and stability:
- Falls become a greater concern as women age, and fall-related fractures are a serious consequence of poor bone health
- Include balance challenges and single-leg work in programs
- Especially important for clients with bone density concerns
- Progress from stable to unstable surfaces, from bilateral to unilateral exercises
- Functional movements like getting up from the floor, stepping over obstacles, and carrying loads while moving all challenge balance in practical ways
- Consider yoga, Tai Chi, or dedicated balance work as adjuncts to strength training
A brief note on cycle-based training¶
For perimenopausal clients who still have menstrual cycles, you may have heard about "cycle-based training", adjusting training intensity based on menstrual cycle phase.
Some research in young, regularly cycling women suggests:
- The follicular phase (early cycle) may support higher intensity training
- The luteal phase (later cycle) may warrant adjusted intensity if symptoms or recovery are affected
For your perimenopausal clients:
- Cycles are often irregular during perimenopause
- Individual variation is enormous
- A pragmatic approach: encourage clients to notice their own patterns and adjust if needed
- Avoid rigid protocols, listen to the client
For postmenopausal clients, cycle-based considerations don't apply since menstrual cycles have stopped.
Common training mistakes¶
The longevity protocol identifies common mistakes women make during this transition:
- Avoiding heavy weights. Many women shy away from lifting heavy, missing the stimulus needed for bone and muscle maintenance
- Excessive cardio without strength training. Cardio alone won't preserve muscle or stimulate bone
- Not adjusting for hormonal changes. Ignoring recovery needs or symptom impacts
- Under-recovering. Not accounting for the sleep disruption that often accompanies menopause
- All-or-nothing thinking. Abandoning exercise entirely when symptoms are challenging
Coaching in practice: When cardio "stops working"¶
The scenario: A client in her late 40s or 50s says, "I've been doing my usual cardio but it's just not working anymore. I'm gaining weight around my middle and I feel weaker."
What NOT to do:
❌ Tell her that cardio is now "useless" or insist she just needs to eat less and work harder.
Why it doesn't work: It dismisses her experience, oversimplifies what's happening physiologically, and can create shame or all-or-nothing thinking.
What TO do:
✅ Validate her frustration, explain what's changing in clear language, and position strength training as an important addition—not a replacement—for her cardio.
Sample dialogue:
Client: "I've been doing my usual cardio but it's just not working anymore. I'm gaining weight around my middle and I feel weaker."
Coach: "That's really common during menopause, and it can be incredibly frustrating. You're putting in the effort and not getting the same return."
Client: "Exactly. It makes me wonder why I bother."
Coach: "What we see around this stage of life is that as estrogen drops, your body tends to shift where it stores fat, and you lose muscle faster than before. Cardio is still great for your heart and overall health, but it doesn't give your muscles or bones the kind of challenge they need to stay strong."
Client: "So what should I do—stop cardio?"
Coach: "You don't have to stop at all. I'd suggest we add strength training: real resistance work, not just light weights. Your body needs that stimulus to maintain muscle and keep bones strong. We can keep some cardio for heart health and add two or three strength sessions a week, starting right where you are and building gradually. How does that sound?"
Client: "That actually feels doable. I'd like to feel strong again."
[CHONK: Nutrition for Female Hormonal Health]
Nutrition during the menopause transition¶
Nutrition plays a supporting role during menopause. It won't eliminate symptoms, but it can help preserve muscle, support bone health, and influence body composition changes.
Protein: More important than ever¶
As women age and estrogen declines, the body becomes more "anabolic resistant." It requires more protein to stimulate muscle protein synthesis.
Targets:
- Aim for 1.0-1.2 grams of protein per kilogram of body weight daily (some evidence suggests up to 1.6 g/kg for active individuals)
- Distribute protein across meals: aim for 25-35 grams per meal, particularly if muscle preservation is a priority.
- Research shows women consuming higher protein intakes have better physical function and higher relative muscle mass
Practical strategies to increase protein:
- Prioritize protein at each meal: make it the anchor of the plate.
- Include protein-rich snacks if needed to meet targets (Greek yogurt, cottage cheese, jerky, hard-boiled eggs)
- Consider protein distribution throughout the day rather than loading at dinner
- Track for a few days to get a reality check. Many people overestimate their protein intake.
Practical note: One of the most common mistakes women make during menopause is under-eating protein. A client doing great on 0.8 g/kg in her 30s may need more in her 50s. Don't assume her current intake is adequate. Actually calculate it.
Bone health nutrition¶
Calcium:
- Target: approximately 1000-1200 mg daily from food and supplements combined
- Food sources: dairy, fortified plant milks, canned fish with bones, leafy greens, tofu
- If supplementing, split doses (≤500-600 mg at a time) improve absorption
- Very high supplemental calcium doses may carry cardiovascular concerns. Favor food-first approaches
Vitamin D:
- Essential for calcium absorption and bone health
- Many postmenopausal women have insufficient vitamin D
- Target: 800-2000 IU daily, depending on blood levels and sun exposure
- Important to ensure sufficiency before or alongside any osteoporosis treatment
Vitamin K2:
- Plays a role in directing calcium to bones
- Found in fermented foods, some cheeses, and egg yolks
- Often included in bone health supplements
Body composition challenges¶
Women often experience frustrating body composition changes during menopause. Weight gain, particularly around the abdomen, can occur despite no changes in eating or exercise.
What's happening:
- Hormonal shifts favor central fat storage
- Lean mass decline reduces metabolic rate
- Sleep disruption can affect appetite hormones
- Stress and life circumstances often peak during midlife
Evidence-based approach:
- Focus on body composition, not just scale weight. The scale may not move much even as body composition improves
- Preserve muscle through resistance training and protein (this is non-negotiable)
- Moderate calorie reduction if needed (500-750 kcal/day deficit); guidelines suggest targeting 5-10 percent weight loss over about 6 months
- Avoid very low calorie diets that sacrifice muscle. Muscle loss worsens the underlying metabolic challenges
- Set realistic expectations. Slow, sustainable change beats rapid weight cycling
- Consider that some body composition change is normal and not entirely preventable
The protein leverage hypothesis suggests that when protein intake is inadequate, the body may drive overconsumption of fats and carbohydrates to meet protein needs. Adequate protein may help with appetite regulation. Another reason why protein should be the first priority.
What to tell clients about weight changes:
Many women feel they're "doing everything right" but gaining weight. Validate this frustration. It's real. But also help them understand:
- Some change is hormonal and not fully controllable through diet and exercise
- Body composition matters more than scale weight
- Maintaining current weight while improving body composition is a win
- The goal is long-term metabolic health, not short-term scale victories
Iron considerations¶
An interesting shift happens after menopause: iron needs decrease once menstrual bleeding stops.
- Premenopausal women need more iron due to menstrual losses
- Postmenopausal women's iron needs drop to the same level as men
- Iron supplementation is rarely needed after menopause unless testing shows deficiency
- Excess iron can be harmful. Don't supplement without testing
Other key nutrients¶
Magnesium:
- Supports bone health, sleep, and muscle function
- Many women don't meet recommendations
- Food sources: nuts, seeds, whole grains, leafy greens
Omega-3 fatty acids:
- Support cardiovascular health
- May have anti-inflammatory effects
- Found in fatty fish, walnuts, flaxseeds
- Supplementation of 2-3 g EPA/DHA daily often recommended for those who don't eat fish regularly
Time-restricted eating considerations¶
Some women find time-restricted eating (TRE) helpful for weight management. But during menopause, some caution is warranted:
- Ensure protein targets are met within the eating window
- Avoid aggressive fasting that could compromise muscle
- Some women find symptoms (particularly sleep or mood) worsen with extended fasting
- If trying TRE, monitor how you feel and adjust accordingly
- 12-14 hour overnight fasts are generally gentler than longer windows
A note on phytoestrogens¶
Phytoestrogens—plant compounds with weak estrogen-like activity found in soy, flaxseeds, and other foods—are sometimes promoted for menopause symptoms.
What the evidence shows:
- Cochrane review found no significant benefit over placebo for hot flashes
- Some mechanistic research suggests potential benefits for bone and metabolic health
- Effects, if any, appear small
- Generally safe as part of a balanced diet
- Not a replacement for medical treatment when symptoms are significant
Coaching in practice: Addressing weight gain concerns¶
The scenario: A client says, "I'm doing everything the same as I used to and I just keep gaining weight. Nothing works anymore."
What NOT to do:
❌ Assume she's "cheating" on her plan, or tell her she just needs to try a very low calorie diet or do even more cardio.
Why it doesn't work: It ignores the real physiological changes of menopause, increases shame, and often leads to unsustainable, all-or-nothing efforts.
What TO do:
✅ Validate her experience, explain what's changing, and focus on protein, strength training, and realistic expectations about the pace and extent of change.
Sample dialogue:
Client: "I'm doing everything the same as I used to and I just keep gaining weight. Nothing works anymore."
Coach: "I hear you. That's one of the most frustrating parts of this stage of life. You're putting in effort and your body isn't responding the way it used to."
Client: "Exactly. It makes me feel like my body is broken."
Coach: "Your body isn't broken, but it is changing how it processes and stores energy. Hormonal shifts around menopause tend to favor more fat around the abdomen, and at the same time, most women lose muscle, which can lower metabolic rate. On top of that, sleep and stress can shift appetite and cravings. So you're not imagining this."
Client: "So is there anything I can actually do?"
Coach: "There are a few things that can genuinely help, even if they don't make the scale behave exactly like it did in your 30s. First, we make sure you're getting enough protein—that's the number one thing I see women under-do. Second, strength training becomes even more important to maintain muscle and metabolism. Third, we work on expectations: the scale might move more slowly than it used to, but we can absolutely improve your body composition and how you feel in your body."
Client: "That feels more realistic. Where should we start?"
Coach: "Let's pick one place that feels doable—maybe adding a bit more protein to breakfast, or starting two short strength sessions per week. We can build from there and adjust based on how your body responds."
[CHONK: Coaching Women Through Hormonal Transitions]
Staying in scope while providing real support¶
This is where everything comes together. You understand the physiology, you know about HRT, and you have training and nutrition strategies. Now, how do you coach effectively while staying firmly within scope?
What coaches CAN do¶
Education and information:
- Explain what happens during menopause in general terms
- Share that evidence on various interventions exists
- Help clients understand what questions to ask their healthcare providers
- Normalize the experience. Menopause is a biological transition, not a disease
Lifestyle support:
- Design appropriate training programs
- Provide nutrition guidance within scope
- Support sleep hygiene improvements
- Help with stress management strategies
- Adjust programs based on symptoms and recovery
Care navigation:
- Encourage conversations with healthcare providers
- Suggest when specialist consultation might be helpful
- Help clients prepare for medical appointments
- Support implementation of medical recommendations
Emotional support:
- Listen without judgment
- Validate the challenges of this transition
- Provide consistency and encouragement
- Help clients maintain perspective
What coaches CANNOT do¶
Medical practice:
- Diagnose conditions (including menopause itself)
- Recommend for or against HRT
- Suggest specific medications, formulations, or doses
- Interpret lab results
- Advise on starting, stopping, or adjusting medical treatments
Testing interpretation:
- Coaches cannot interpret hormone tests
- If a client shows you lab results, you can help them understand what the tests measure in general terms, but interpretation belongs to their healthcare provider
When to refer¶
These situations warrant medical referral:
Urgent (immediate medical attention):
- Any vaginal bleeding after menopause (postmenopausal bleeding is a red flag)
- Severe or worsening pelvic pain, especially with fever
- Signs of serious illness
Prompt medical consultation:
- Symptoms significantly affecting quality of life (hot flashes disrupting sleep night after night, mood changes interfering with relationships or work)
- Symptoms not responding to lifestyle measures after a reasonable trial
- Client interested in discussing HRT or other medical treatments
- Suspected premature menopause (before age 40). These clients need specialist evaluation
- History of hormone-sensitive cancers, blood clots, or significant cardiovascular disease. Complex medical decision-making required
- Concerning bone density results (osteopenia or osteoporosis)
- Depression or anxiety that's more than mild or situational. Screen for mental health needs
- Genitourinary symptoms causing significant distress (vaginal therapies may help)
- Persistent bleeding irregularities that haven't been evaluated
- Client with complex medical conditions affecting lifestyle recommendations
What to say:
"What you're describing sounds like something worth discussing with your doctor. They can evaluate whether there are medical options that might help. I'm here to support you with the lifestyle side, but this is beyond what I can address as a coach."
Supporting clients on HRT¶
Some of your clients will be taking HRT. How do you support them?
Do:
- Continue providing lifestyle coaching
- Support healthy habits that matter regardless of HRT status
- Ask how they're doing in general
- Adjust training if they mention side effects affecting their workouts
Don't:
- Comment on whether they should be on HRT
- Offer opinions about their formulation or dose
- Suggest changes to their HRT
- Express skepticism or enthusiasm about their medical treatment
Your role is the same as with any client on medication: support lifestyle factors, stay in your lane.
Supporting clients not on HRT¶
Some clients will choose not to use HRT, or it may not be appropriate for them. Support them too:
Do:
- Respect their decision
- Focus on lifestyle factors that can help
- Maintain realistic expectations: lifestyle can help but may not eliminate symptoms
- Acknowledge that some discomfort may persist
Don't:
- Push them toward HRT
- Imply they're "missing out"
- Guarantee that lifestyle changes will resolve their symptoms
Managing expectations¶
Honest expectation-setting is important:
- Menopause is normal, not a disease to be cured
- Some symptoms may persist despite best efforts
- Progress may be slower than in earlier years
- The goal is thriving within a changing body, not returning to "before"
- Consistency beats perfection
Deep Health integration¶
Remember that menopause affects all dimensions of Deep Health:
| Dimension | Consideration |
|---|---|
| Physical | Symptoms, body composition, bone health, cardiovascular risk |
| Emotional | Mood changes, identity shifts, frustration with body changes |
| Mental | Cognitive changes, confidence, self-perception |
| Environmental | Sleep environment, temperature management |
| Relational | Impact on relationships, communication with partners, changing roles |
| Existential | Life transitions, meaning-making, "who am I now?" |
A client struggling with menopause symptoms may also be dealing with aging parents, children leaving home, career shifts, and relationship changes. The physical symptoms exist within a larger life context.
How Deep Health informs your coaching:
Physical: This is your primary domain. Training, nutrition, sleep hygiene, and movement all fall within coaching scope.
Emotional: Validate feelings. Mood changes are real and partly hormonal. You can support coping strategies and stress management. But if mood changes suggest clinical depression or anxiety, refer to mental health professionals.
Mental: "Brain fog" is frustrating but usually resolves. Reassure clients that cognitive function typically remains within normal limits. Support good sleep and stress management, which influence cognition.
Environmental: Help with practical adjustments: sleep environment for night sweats, temperature control strategies, ensuring access to movement opportunities.
Relational: Acknowledge that relationships may be affected. Encourage communication with partners. Recognize that midlife often involves caregiving responsibilities that affect time and energy.
Existential: Menopause often coincides with existential questions: "What do I want from this next phase of life?" You can create space for these conversations without providing therapy. Help clients connect their health behaviors to their larger values and goals.
The midlife context¶
Menopause doesn't happen in isolation. This life stage often brings:
- Children leaving home (or returning)
- Aging parents requiring care
- Career transitions (peak demands or contemplating change)
- Relationship shifts (divorce, empty nest adjustments, loss of loved ones)
- Health concerns beyond menopause (both the client's own and family members')
- Financial pressures (college costs, retirement planning)
If you're reading this and thinking, "No wonder my clients feel overwhelmed" (or maybe you do too), that's a completely normal reaction.
These stressors affect hormones, sleep, eating, and exercise adherence. A coaching approach that only addresses physical symptoms misses the larger picture. Use the Deep Health model to understand your client's full context.
Coaching in practice: Supporting a client through early menopause¶
The scenario: Sarah, 48, reports that her periods have become irregular over the past year. She's experiencing hot flashes (4-5 per day), sleep disruption (waking 2-3 times nightly), and has gained about 8 pounds despite no changes in eating. She says she feels "foggy" and has less energy than she used to. She's frustrated and says she "feels like she's falling apart."
Sarah asks if she should try HRT.
What NOT to do:
❌ Tell her, "This is definitely perimenopause; you should go on HRT" or suggest specific hormones or doses.
Why it doesn't work: That crosses into diagnosis and medical prescribing, which are outside your scope, and it oversimplifies what might be going on.
What TO do:
✅ Validate her experience, acknowledge that her symptoms are common in the menopause transition, be clear about your scope boundaries, encourage medical evaluation, and offer concrete lifestyle support.
Sample dialogue:
Sarah: "My periods are all over the place, I'm having hot flashes all day and night, I've gained eight pounds without changing anything, and I feel foggy all the time. I honestly feel like I'm falling apart. Do you think I should try HRT?"
Coach: "I can hear how overwhelming this feels, and it makes sense you'd be frustrated. A lot of what you're describing—irregular periods, hot flashes, sleep disruption, weight changes, and brain fog—are really common during the transition into menopause. That doesn't make them any less challenging, but you're definitely not alone in this."
Sarah: "It's almost a relief to hear that, but I still don't know what to do."
Coach: "About HRT specifically, that's something I can't advise you on. It's a medical decision that depends on your individual health history and risk factors. What I would encourage is having a conversation with your doctor or a menopause specialist so they can help you understand your options."
Sarah: "Okay. I can do that. But I also just want to feel better day to day."
Coach: "Absolutely. What I can do is work with you on the lifestyle pieces that genuinely help during this transition—things like your sleep environment and habits, nutrition, especially making sure you're getting enough protein, and adjusting your exercise approach so it supports you instead of draining you. These won't necessarily eliminate every symptom, but they can make a real difference in how you feel."
Sarah: "That sounds helpful. Where should we start?"
Coach: "How about we start by looking at what's happening with your sleep and recovery? If we can get you sleeping a bit better, that often helps with mood, energy, and even appetite. We can work on that while you're talking with your doctor about the medical side."
Key elements:
- Validated her experience
- Named what's likely happening without diagnosing
- Was clear about scope boundaries
- Encouraged medical consultation
- Offered concrete support within scope
- Didn't promise lifestyle changes would fix everything
[CHONK: Study Guide Questions]
Study guide questions¶
These questions help you think through the material and prepare for the chapter exam. They're optional, but we recommend answering at least a few as part of your active learning process.
-
What is the difference between perimenopause and menopause? Why does this distinction matter for coaching?
-
A client asks you, "Is HRT safe?" How would you respond in a way that's informative but stays within scope?
-
Why might postmenopausal women need higher resistance training volumes than premenopausal women to achieve the same muscle-building response?
-
What are three red flags that would prompt you to refer a menopausal client for immediate medical attention?
-
How would you explain to a client why protein needs increase during menopause?
-
A client is frustrated that her cardio routine isn't preventing weight gain like it used to. What would you explain, and what would you suggest?
Self-reflection questions:
-
If you're a woman approaching or in menopause: How much strength training are you currently doing? Does it match the recommendations in this chapter?
-
Regardless of your gender, how can understanding hormonal transitions help you be a more empathetic and effective coach—or advocate for the women in your life?
Chapter exam¶
Question 1: What defines menopause?
a) The first hot flash
b) Irregular periods for 6 months
c) 12 consecutive months without a menstrual period
d) Low estrogen on a blood test
Question 2: A client asks, "Should I take HRT?" What's the most appropriate response?
a) "Yes, the evidence shows it's beneficial when started early."
b) "No, it's too risky."
c) "That's a medical decision for you and your healthcare provider. I can support you with lifestyle factors either way."
d) "Let me look at your hormone levels first."
Question 3: Which exercise modality is MOST important for preserving muscle mass during menopause?
a) Walking
b) Yoga
c) Resistance training
d) Swimming
Question 4: Why do protein needs increase during menopause?
a) Estrogen increases protein breakdown
b) The body becomes more anabolic resistant, requiring more protein to stimulate muscle synthesis
c) Menopause causes protein deficiency
d) Protein helps reduce hot flashes
Question 5: A postmenopausal client reports vaginal bleeding. What should you do?
a) Recommend she increase fiber intake
b) Suggest she wait to see if it continues
c) Refer her for urgent medical evaluation. This is a red flag
d) Adjust her training program
Question 6: What is the "timing hypothesis" related to HRT?
a) HRT should only be taken in the morning
b) HRT should be taken for exactly 5 years
c) Starting HRT within about 10 years of menopause may have a more favorable benefit-risk profile than starting later
d) All women should start HRT at age 50
Question 7: Which statement about testosterone therapy for women is accurate?
a) It's recommended for energy and well-being
b) It's only indicated for diagnosed hypoactive sexual desire disorder after other causes are excluded, under medical supervision
c) It should be taken by all postmenopausal women
d) It's unsafe for women
Question 8: A menopausal client is only doing cardio and complains of weight gain and feeling weaker. What's the most important addition to her program?
a) More cardio
b) Longer fasting periods
c) Resistance training
d) Meditation
Question 9: How much calcium should postmenopausal women aim for daily?
a) 400-500 mg
b) 1000-1200 mg
c) 2000-2500 mg
d) As little as possible
Question 10: Which is within a coach's scope of practice?
a) Recommending a specific HRT formulation
b) Interpreting hormone lab results
c) Designing a strength training program and encouraging a medical consultation for symptoms
d) Advising when to start or stop HRT
Question 11: What's the most effective treatment for vasomotor symptoms (hot flashes)?
a) Exercise. Research consistently shows it eliminates hot flashes
b) Phytoestrogen supplements
c) Hormone replacement therapy (a medical decision)
d) Protein supplements
Question 12: When should you refer a menopausal client to a specialist?
a) Never. Coaches handle all menopause concerns
b) When symptoms significantly affect quality of life, when the client is interested in HRT, or when red flags appear
c) Only after trying every possible lifestyle intervention
d) Only if she's over 60
[CHONK: Works Cited]
Works cited¶
References¶
-
Office on Women's Health. Menopause basics. U.S. Department of Health & Human Services; 2025. https://womenshealth.gov/menopause/menopause-basics
-
Wegrzynowicz AK, Walls AC, Godfrey M, Beckley A. Insights into Perimenopause: A Survey of Perceptions, Opinions on Treatment, and Potential Approaches. Women. 2025;5(1):4. doi:10.3390/women5010004
-
DELAMATER L, SANTORO N. Management of the Perimenopause. Clinical Obstetrics & Gynecology. 2018;61(3):419-432. doi:10.1097/grf.0000000000000389
-
Paramsothy P, Harlow SD, Nan B, Greendale GA, Santoro N, Crawford SL, et al. Duration of the menopausal transition is longer in women with young age at onset: the multiethnic Study of Women's Health Across the Nation. Menopause. 2017;24(2):142-149. doi:10.1097/gme.0000000000000736
-
Todorova L, Bonassi R, Guerrero Carreño FJ, Hirschberg AL, Yuksel N, Rea C, et al. Prevalence and impact of vasomotor symptoms due to menopause among women in Brazil, Canada, Mexico, and Nordic Europe: a cross-sectional survey. Menopause. 2023;30(12):1179-1189. doi:10.1097/gme.0000000000002265
-
Baker FC, Lampio L, Saaresranta T, Polo-Kantola P. Sleep and Sleep Disorders in the Menopausal Transition. Sleep Medicine Clinics. 2018;13(3):443-456. doi:10.1016/j.jsmc.2018.04.011
-
Salari N, Hasheminezhad R, Hosseinian-Far A, Rasoulpoor S, Assefi M, Nankali S, et al. Global prevalence of sleep disorders during menopause: a meta-analysis. Sleep and Breathing. 2023;27(5):1883-1897. doi:10.1007/s11325-023-02793-5
-
Conde DM, Verdade RC, Valadares ALR, Mella LFB, Pedro AO, Costa-Paiva L. Menopause and cognitive impairment: A narrative review of current knowledge. World Journal of Psychiatry. 2021;11(8):412-428. doi:10.5498/wjp.v11.i8.412
-
Nair AR, Pillai AJ, Nair N. Cardiovascular Changes in Menopause. Current Cardiology Reviews. 2021;17(4). doi:10.2174/1573403x16666201106141811
-
Rani J, Swati S, Meeta M, Singh SH, Tanvir T, Madan A. Postmenopausal Osteoporosis: Menopause Hormone Therapy and Selective Estrogen Receptor Modulators. Indian Journal of Orthopaedics. 2023;57(S1):105-114. doi:10.1007/s43465-023-01071-6
-
Nudy M, Chinchilli VM, Foy AJ. A systematic review and meta-regression analysis to examine the ‘timing hypothesis’ of hormone replacement therapy on mortality, coronary heart disease, and stroke. IJC Heart & Vasculature. 2019;22:123-131. doi:10.1016/j.ijcha.2019.01.001
-
The North American Menopause Society. The 2022 Hormone Therapy Position Statement. Menopause; 2022. https://pubmed.ncbi.nlm.nih.gov/35797481/
-
Abenhaim HA, Suissa S, Azoulay L, Spence AR, Czuzoj-Shulman N, Tulandi T. Menopausal Hormone Therapy Formulation and Breast Cancer Risk. Obstetrics & Gynecology. 2022;139(6):1103-1111. doi:10.1097/aog.0000000000004723
-
Asi N, Mohammed K, Haydour Q, Gionfriddo MR, Vargas OLM, Prokop LJ, et al. Progesterone vs. synthetic progestins and the risk of breast cancer: a systematic review and meta-analysis. Systematic Reviews. 2016;5(1). doi:10.1186/s13643-016-0294-5
-
Oliveira GMMd, Almeida MCCd, Arcelus CMA, Espíndola L, Rivera MAM, Silva-Filho ALd, et al. Brazilian Guideline on Menopausal Cardiovascular Health – 2024. Revista Brasileira de Ginecologia e Obstetrícia. 2024;46. doi:10.61622/rbgo/2024rbgo100
-
Agostini D, Donati Zeppa S, Lucertini F, Annibalini G, Gervasi M, Ferri Marini C, et al. Muscle and Bone Health in Postmenopausal Women: Role of Protein and Vitamin D Supplementation Combined with Exercise Training. Nutrients. 2018;10(8):1103. doi:10.3390/nu10081103
-
Whitman PW, Alexander CJ, Kaluta L, Burt LA, Gabel L. Does exercising during peri- or early post-menopause prevent bone and muscle loss: A systematic review. Bone. 2025;201:117650. doi:10.1016/j.bone.2025.117650
-
Khalafi M, Habibi Maleki A, Sakhaei MH, Rosenkranz SK, Pourvaghar MJ, Ehsanifar M, et al. The effects of exercise training on body composition in postmenopausal women: a systematic review and meta-analysis. Frontiers in Endocrinology. 2023;14. doi:10.3389/fendo.2023.1183765
-
Kopp D, et al.. Resistance training alters body composition in middle-aged women depending on menopause. BMC Women's Health; 2023. https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-023-02671-y
-
Qian J, Sun S, Wang M, Sun Y, Sun X, Jevitt C, et al. The effect of exercise intervention on improving sleep in menopausal women: a systematic review and meta-analysis. Frontiers in Medicine. 2023;10. doi:10.3389/fmed.2023.1092294
-
Daley A, Stokes-Lampard H, MacArthur C. Exercise for vasomotor menopausal symptoms. Cochrane Database of Systematic Reviews. 2011. doi:10.1002/14651858.cd006108.pub3
-
Nahas PC, Rossato LT, Martins FM, Souza AP, de Branco FMS, Carneiro MAS, et al. Moderate Increase in Protein Intake Promotes a Small Additional Improvement in Functional Capacity, But Not in Muscle Strength and Lean Mass Quality, in Postmenopausal Women Following Resistance Exercise: A Randomized Clinical Trial. Nutrients. 2019;11(6):1323. doi:10.3390/nu11061323
-
Khanal P, He L, Degens H, Stebbings GK, Onambele-Pearson GL, Williams AG, et al. Dietary Protein Requirement Threshold and Micronutrients Profile in Healthy Older Women Based on Relative Skeletal Muscle Mass. Nutrients. 2021;13(9):3076. doi:10.3390/nu13093076
-
Gregson CL, Armstrong DJ, Avgerinou C, Bowden J, Cooper C, Douglas L, et al. The 2024 UK clinical guideline for the prevention and treatment of osteoporosis. Archives of Osteoporosis. 2025;20(1). doi:10.1007/s11657-025-01588-3
-
Korean Society of Menopause. The 2024 Guidelines for Osteoporosis. J Menopausal Med; 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC11103071/
-
Lumsden MA, Davies M, Sarri G, for the Guideline Development Group for Menopause: Diagnosis and Management (NICE Clinical Guideline No. 23). Diagnosis and Management of Menopause. JAMA Internal Medicine. 2016;176(8):1205. doi:10.1001/jamainternmed.2016.2761
-
Shokri-Ghadikolaei A, Bakouei F, Delavar MA, Azizi A, Sepidarkish M. Effects of health coaching on menopausal symptoms in postmenopausal and perimenopausal women. Menopause. 2022;29(10):1189-1195. doi:10.1097/gme.0000000000002050
-
Wierman ME, Arlt W, Basson R, Davis SR, Miller KK, Murad MH, et al. Androgen Therapy in Women: A Reappraisal: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism. 2014;99(10):3489-3510. doi:10.1210/jc.2014-2260
-
Fenton A. Weight, Shape, and Body Composition Changes at Menopause. Journal of Mid-life Health. 2021;12(3):187-192. doi:10.4103/jmh.jmh_123_21