Unit 3: Advanced Topics & Disease Prevention¶
Chapter 3.19: Cancer Risk Reduction¶
[CHONK: 1-minute summary]
What you'll learn in this chapter:
- Why cancer belongs in a longevity certification. And how to discuss it without fear-mongering
- The empowering truth: 30-50% of cancer cases are linked to modifiable lifestyle factors
- Which lifestyle factors have the strongest evidence for reducing cancer risk
- How metabolic health connects to cancer prevention (connecting your Unit 2 learning)
- Cancer screening basics for educational awareness, without recommending specific tests
- When genetics matter and when to refer clients for genetic counseling
- Scope-safe language patterns for cancer-related coaching conversations
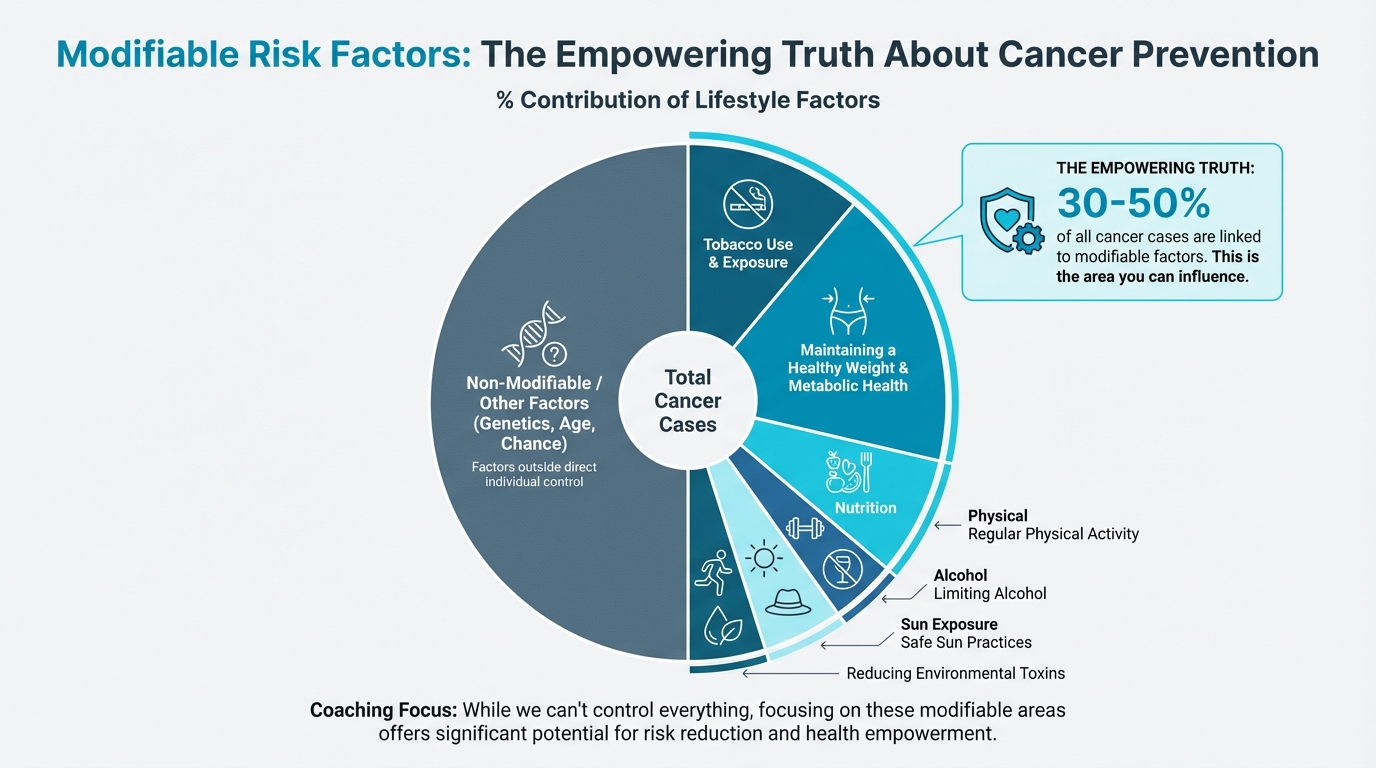
Figure: % contribution of lifestyle factors
The big idea: Cancer is an emotionally charged topic. Your clients may fear it, have family members affected by it, or wonder what they can do to lower their risk. The empowering news is that a substantial portion of cancer risk is within their control. This chapter equips you to discuss cancer prevention through a lens of empowerment, not fear. It focuses on what clients CAN do while maintaining crystal-clear boundaries about what requires physician guidance. You're not here to diagnose, screen, or recommend tests. You're here to help clients build the lifestyle foundations that research shows can meaningfully reduce risk.
[CHONK: Cancer: What Coaches Need to Know]
Why cancer is in this certification¶
If you're thinking, "Wait, cancer? Isn't that outside coaching scope?" you're asking the right question.
You're correct that diagnosing cancer, recommending screening tests, and interpreting results are firmly outside your scope. But here's what isn't outside your scope: helping clients build the lifestyle habits that research consistently links to lower cancer risk.
Cancer is the second leading cause of death globally. It touches nearly every family. And your clients are thinking about it, whether they tell you or not.
The good news is remarkable: research from the World Health Organization and major cancer research institutions consistently finds that 30-50% of all cancer cases are linked to modifiable risk factors. That's not a typo. Up to half of cancers could potentially be prevented through lifestyle changes. If that number feels both hopeful and a bit overwhelming, that's normal.
In the United States, the American Cancer Society estimates that approximately 40% of cancer cases and nearly 50% of cancer deaths among adults are attributable to modifiable factors. The largest single contributor is tobacco, but even after excluding smoking, about 1 in 5 U.S. cancers are linked to excess body weight, physical inactivity, unhealthy diet, and alcohol.
This is where you come in. The same fundamentals you've been coaching throughout this certification—regular physical activity, healthy body composition, quality nutrition, adequate sleep, stress management—are also cancer prevention strategies. (Which is actually pretty encouraging.)
The empowerment frame¶
Before we go any further, let's establish the most important principle for this entire chapter:
Empowering, not fear-inducing.
Cancer conversations can easily slide into fear territory. Media coverage emphasizes frightening statistics. Clients may have lost loved ones or carry their own worries. Your job is to be a steady presence who grounds these conversations in what people can actually do.
Key phrases to internalize:
- "What you CAN control..."
- "Reducing risk, not eliminating risk"
- "The research shows meaningful reductions when..."
- "This is something to discuss with your doctor"
What we avoid:
- "If you don't do X, you might get cancer"
- Guarantees or false reassurance
- Minimizing legitimate concerns
- Making screening recommendations
What coaches CAN and CANNOT do¶
Let's be crystal clear about boundaries. Return to what you learned in Chapter 1.5.
You CAN:
- Share evidence-based information about lifestyle factors and cancer risk
- Help clients implement health behaviors (exercise, nutrition, sleep) that happen to reduce cancer risk
- Support clients emotionally when cancer is on their mind
- Encourage clients to have screening discussions with their healthcare providers
- Help clients follow through on recommendations their doctors have already made
You CANNOT:
- Recommend specific screening tests ("You should get a colonoscopy")
- Interpret screening results or lab work
- Provide guidance on cancer treatment
- Suggest specific protocols for "cancer prevention"
- Determine whether someone's symptoms warrant concern
The line is simple: education and lifestyle support = yes. Medical recommendations = no.
When in doubt, the phrase is always: "That's definitely something to discuss with your doctor."
[CHONK: Modifiable Risk Factors]
The lifestyle factors you can actually address¶
Here's where the empowerment gets concrete. Let's walk through the major modifiable risk factors for cancer, ranked roughly by the strength of evidence and magnitude of impact.
Tobacco: The #1 modifiable factor¶
We'll address this briefly because you likely know it already, but the numbers are worth stating: cigarette smoking alone accounts for approximately 20% of all U.S. cancer cases and about 30% of cancer deaths.
Smoking causes cancers of the lung, mouth, throat, esophagus, stomach, kidney, bladder, pancreas, and more. The carcinogenic mechanisms are multiple: direct DNA damage, chronic inflammation, and impaired immune function.
The coaching angle: If you have clients who smoke, smoking cessation support is likely the single most impactful intervention you could assist with. But recognize that nicotine addiction is complex, and referral to cessation programs, behavioral health, or their physician may be appropriate. Your role is supportive, not prescriptive.
Alcohol: The carcinogen many don't know about¶
This one surprises people. The International Agency for Research on Cancer (IARC)—the cancer research arm of the World Health Organization—classifies alcohol as a Group 1 carcinogen, the highest classification for substances known to cause cancer in humans. This puts it in the same category as tobacco.
What the research shows:
Alcohol has causal links to cancers of the oral cavity, pharynx, larynx, esophagus, liver, colorectum, and female breast. The mechanisms are well-understood: when you drink alcohol, your body metabolizes it to acetaldehyde, a compound that directly damages DNA, causes mutations, and interferes with DNA repair.
The dose-response relationship is clear and begins at low levels. Research shows:
- Light drinking (less than one drink per day) significantly increases risk for esophageal, colorectal, and breast cancers
- Each additional standard drink per day increases postmenopausal breast cancer risk by approximately 12%
- Heavy drinking raises head and neck cancer risk approximately 5-fold compared to non-drinkers
The "no safe level" evidence:
Here's where we apply our "island of sanity" principle: sharing what the evidence actually shows, not what people want to hear.
Current scientific consensus, including from the WHO, is that no level of alcohol consumption is safe for cancer risk. Risk increases continuously from the first drink. About half of alcohol-attributable cancers in Europe arise from light to moderate consumption.
This doesn't mean every client who has an occasional drink is at imminent risk. It means that from a pure cancer risk standpoint, less is better, and none is best. How clients weigh that against other life factors is their choice to make.
What this means for your client:
When clients ask about alcohol and health, you can share this evidence factually. Many people genuinely don't know alcohol is classified as a carcinogen. You're not telling them what to do. You're ensuring they have accurate information for their own decisions.
A scope-safe conversation might sound like: "The research on alcohol and cancer risk might surprise you. Alcohol is actually classified as a known carcinogen by the WHO. The risk increases with amount, and research suggests there isn't a level that's 'safe' from a cancer perspective. How you balance that information with other factors in your life is your call. If you want to discuss reducing your intake, I'm happy to help with that process."
Body composition and visceral fat¶
You covered metabolic health extensively in Unit 2. Here's how it connects to cancer.
Excess body fat, particularly visceral (abdominal) fat, is linked to increased risk for at least 13 types of cancer. These include breast (postmenopausal), colorectal, endometrial, esophageal, kidney, liver, gallbladder, stomach, pancreatic, ovarian, thyroid, multiple myeloma, and meningioma.
The CDC notes that these obesity-linked cancers account for approximately 40% of all U.S. cancer diagnoses each year.
Mechanisms matter:
Why does excess fat increase cancer risk? The pathways you learned in Unit 2 are directly relevant:
| Mechanism | How It Promotes Cancer |
|---|---|
| Chronic inflammation | Visceral fat tissue becomes infiltrated with immune cells that release inflammatory cytokines (TNF-α, IL-6, IL-1β), creating a tumor-promoting environment |
| Hyperinsulinemia | Elevated insulin and insulin-like growth factor (IGF-1) activate growth pathways (PI3K/Akt/mTOR) that promote cell proliferation and inhibit apoptosis |
| Adipokine imbalance | Increased leptin promotes proliferative signaling; decreased adiponectin removes its tumor-suppressive effects |
| Elevated estrogens | Adipose tissue contains aromatase, which converts androgens to estrogens, particularly relevant for hormone-sensitive cancers like breast and endometrial |
If these pathways and acronyms feel complicated, that's okay. You don't need to memorize every mechanism; the key takeaway is that less visceral fat and better metabolic health mean lower cancer risk.
Risk varies by site:
Meta-analyses provide specific risk estimates. Compared to normal weight:
- Endometrial cancer risk increases approximately 76% with overweight/obesity
- Kidney cancer risk increases approximately 50%
- Liver cancer risk increases approximately 52%
- Colorectal cancer risk increases approximately 27%
- Postmenopausal breast cancer risk increases approximately 13%
The good news: weight loss helps:
Studies of bariatric surgery provide the strongest evidence: patients who undergo bariatric surgery show a 38% reduction in overall cancer risk, with particularly large reductions for endometrial (62% lower), liver (65% lower), and colorectal (37% lower) cancers.
Lifestyle-based weight loss shows similar direction, though the magnitude is harder to quantify because sustained large weight loss is difficult to achieve through lifestyle alone. The Look AHEAD trial of intensive lifestyle intervention showed a trend toward 16% lower obesity-related cancer incidence, though the study wasn't powered to detect statistical significance for cancer endpoints.
What this means for your client:
The metabolic health work you're already helping clients with IS cancer prevention work. When you help someone improve body composition, reduce visceral fat, and improve metabolic markers, you're simultaneously addressing cancer risk.
Physical activity¶
If you could bottle the cancer-prevention effects of exercise and sell it as a pill, it would be worth billions.
What the research shows:
Higher physical activity is consistently associated with lower incidence of multiple cancers. The benefits appear across numerous cancer sites:
| Cancer Site | Risk Reduction (High vs. Low Activity) |
|---|---|
| Colon | ~7-25% lower risk |
| Breast | ~10-20% lower risk |
| Endometrial | ~18% lower risk |
| Liver | ~17% lower risk |
| Kidney | Variable, substantial reductions |
| Lung | ~12-22% lower risk |
| Bladder | ~32% lower risk |
Meeting guideline-level activity (approximately 150-300 minutes per week of moderate activity) is associated with 6-29% lower risk across several cancer types. The benefits appear dose-dependent. More activity generally means more protection, though with diminishing returns at very high levels.
Mechanisms:
Exercise likely reduces cancer risk through multiple pathways:
- Insulin/IGF signaling: Exercise improves insulin sensitivity and reduces circulating insulin and IGF-1
- Inflammation: Regular activity reduces chronic systemic inflammation
- Sex hormones: Exercise can lower circulating estrogens, particularly relevant for breast and endometrial cancer
- Immune function: Exercise enhances immune surveillance
- Direct effects: Myokines (muscle-derived signaling molecules) may have anti-tumor properties
Sedentary time matters independently:
Research shows that sedentary behavior increases cancer risk independent of physical activity levels. High sedentary time is associated with:
- 29% higher ovarian cancer risk
- 29% higher endometrial cancer risk
- 25% higher colon cancer risk
This means that even for clients who exercise regularly, reducing prolonged sitting time may provide additional benefit.
What this means for your client:
The exercise programming you're already helping clients with is cancer prevention programming. When you help someone establish consistent physical activity habits, you're simultaneously reducing their cancer risk. This adds another dimension to your motivational conversations. Exercise isn't just about how you look or feel today; it's about your health trajectory over decades.
Diet and inflammation¶
The diet-cancer relationship is complex, and certainty is lower than for the factors above. But several patterns emerge from large-scale research.
What appears protective:
- High fruit and vegetable intake (associated with lower risk for several cancers)
- Fiber intake (particularly for colorectal cancer)
- Dietary patterns rich in whole foods (Mediterranean-style patterns show consistent associations with lower cancer incidence)
What appears to increase risk:
- Processed meat (IARC classifies as Group 1 carcinogen; linked to colorectal cancer)
- Red meat (IARC classifies as Group 2A, probably carcinogenic; linked to colorectal cancer)
- Ultra-processed foods (emerging evidence links higher intake to increased cancer incidence)
- High glycemic load diets (likely through metabolic pathways discussed above)
Important context:
Diet research is challenging. People who eat healthier also tend to have other healthy behaviors, making causation difficult to establish. Effect sizes for individual foods are generally modest compared to factors like smoking, alcohol, and obesity.
The practical takeaway: whole-food dietary patterns that you'd recommend for metabolic health are also the patterns associated with lower cancer risk. You don't need separate "cancer prevention diets". The fundamentals apply.
| Modifiable Risk Factor | Impact on Cancer Risk | Strength of Evidence |
|---|---|---|
| Tobacco | ~20% of all cancers; ~30% of cancer deaths | Very Strong |
| Alcohol | Causes 7+ cancer types; dose-dependent risk from first drink | Very Strong |
| Excess body fat | Linked to 13 cancer types; ~40% of diagnoses are obesity-related cancer types | Strong |
| Physical inactivity | Higher activity = 6-29% lower risk across multiple sites | Strong |
| Diet | Processed meat, low fiber, ultra-processed foods associated with higher risk | Moderate |
| Sun/UV exposure | Major cause of skin cancers (not covered in detail here) | Very Strong |
[CHONK: The Metabolic-Cancer Connection]
Connecting your Unit 2 learning¶
Everything you learned in Unit 2 about metabolic health has direct implications for cancer risk. Let's make those connections explicit.
Insulin, insulin resistance, and cancer¶
Insulin resistance isn't just about diabetes risk. It's a cancer risk factor.
The mechanisms are well-characterized:
- Hyperinsulinemia promotes tumor growth: Elevated insulin activates insulin receptors on cells, triggering growth and proliferation pathways (PI3K/Akt/mTOR, MAPK). Cancer cells often overexpress insulin receptors.
- IGF-1 amplification: Insulin resistance increases bioavailable IGF-1, a potent growth factor that promotes cell division and inhibits apoptosis.
- Fuel supply: High insulin states increase availability of glucose and fatty acids that cancer cells can use for energy and growth.
The epidemiological evidence:
Type 2 diabetes is associated with approximately 10-17% higher overall cancer risk, with particularly elevated risks for pancreatic, liver, and endometrial cancers. People with diabetes have approximately 20-30% higher cancer mortality.
Metabolic syndrome—the cluster of insulin resistance, central obesity, dyslipidemia, and hypertension—is associated with:
- ~2-fold increased risk of endometrial cancer
- Higher recurrence and mortality in breast cancer survivors
- Reduced remaining life expectancy after cancer diagnosis
An important distinction:
Research using genetic techniques (Mendelian randomization) suggests that elevated fasting insulin, not fasting glucose, may be the causal driver for colorectal cancer risk. This aligns with the mechanistic understanding: it's the hyperinsulinemia that matters most, not just blood sugar levels.
Chronic inflammation¶
You learned about inflammation as a metabolic disruptor. It's also a cancer promoter.
Chronic low-grade inflammation, often called "inflammaging", creates an environment where cancer can initiate and progress. The NF-κB and STAT3 signaling pathways, when chronically activated by inflammatory signals, promote tumor survival and growth.
Research estimates that approximately 15-25% of cancers arise from or are promoted by chronic inflammatory conditions.
The sources of chronic inflammation relevant to your coaching work include:
- Visceral adiposity (inflamed fat tissue)
- Poor metabolic health
- Chronic stress
- Poor sleep
- Sedentary behavior
- Diet high in processed foods
If the mechanisms and terminology here feel complex, that's normal; you don't need to remember every pathway, only that chronic inflammation and poor metabolic health can raise cancer risk.
What this means for your client¶
Here's the empowering synthesis: metabolic health coaching IS cancer prevention coaching.
When you help a client:
- Improve insulin sensitivity through exercise and nutrition → you're reducing cancer risk pathways
- Reduce visceral fat → you're reducing inflammation and cancer-promoting signals
- Build muscle mass → you're improving metabolic health and potentially benefiting from myokine effects
- Manage stress and improve sleep → you're reducing inflammatory burden
You don't need to frame it as "cancer prevention" in every conversation. That could be anxiety-provoking for some clients. But you can feel confident that the fundamental work of helping people live healthier lives has implications far beyond what the scale shows.
Coaching in practice: When a client asks about cancer prevention¶
The scenario: A client shares that a close relative has been diagnosed with cancer and asks what they can do to lower their own risk.
Client: "My aunt was just diagnosed with breast cancer. It's got me thinking: what can I do to lower my own risk?"
What NOT to do:
❌ Jump straight into detailed risk calculations or start recommending specific screening tests or genetic panels.
Why this doesn't work: You're not the one to assess their personal medical risk, and making specific medical recommendations steps outside your scope of practice and can increase anxiety.
What TO do:
✅ Treat it as both an emotional moment and a coaching opportunity. Acknowledge the emotion first, then share modifiable risk factors and reinforce appropriate referral.
Coach: "I'm sorry to hear about your aunt. That must be concerning, especially when it's someone close to you." [Pause, acknowledge]
Coach: "I can share what the research shows about modifiable risk factors: the things that are actually within your control. For breast cancer specifically, the evidence points to maintaining a healthy weight, staying physically active, and being thoughtful about alcohol. Those are all things we can work on together."
Coach: "For anything specific to your personal risk given your family history, that's worth discussing with your doctor. They might recommend different screening schedules or want to discuss genetic testing. Would it help to think through what questions you might want to ask them?"
Key takeaways:
- Acknowledge the emotional weight first
- Provide empowering, behavior-focused information
- Maintain clear scope boundaries around risk assessment and testing
- Facilitate the appropriate healthcare conversation
[CHONK: Cancer Screening: Educational Awareness]
What coaches should know about screening¶
Your clients will ask about cancer screening. They'll wonder if they're "up to date," whether they should get tested for something, or what the latest guidelines say.
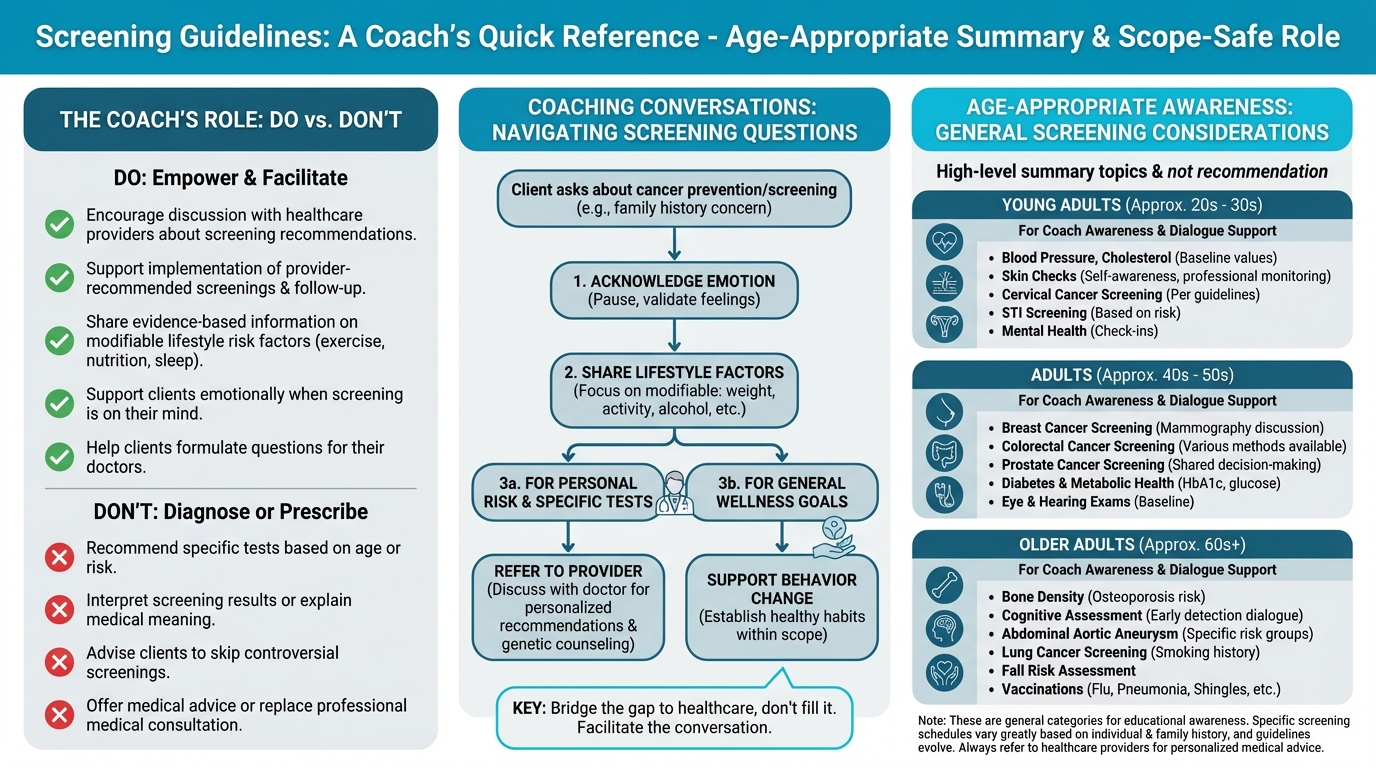
Figure: Age-appropriate screening summary
You are not qualified to recommend specific screening tests. That's physician territory. But having educational awareness helps you support informed conversations.
Overview of screening guidelines¶
The U.S. Preventive Services Task Force (USPSTF) is the primary body that reviews evidence and makes screening recommendations. Their grades range from A (strongly recommend) to D (recommend against), with C (individual decision) and I (insufficient evidence) in between.
Educational overview of common screenings:
| Screening | What It Is | General Population* |
|---|---|---|
| Colonoscopy | A procedure where a physician examines the colon with a camera to detect polyps (precancerous growths) and cancer | USPSTF recommends colorectal screening for adults 45-75 (multiple test options including colonoscopy, stool tests) |
| Mammography | X-ray imaging of breast tissue to detect cancer early | USPSTF recommends biennial mammograms for women 40-74 |
| PSA test | A blood test measuring prostate-specific antigen | USPSTF recommends shared decision-making for men 55-69; recommends against routine screening for men 70+ |
| Cervical (Pap/HPV) | Cervical cell sampling to detect precancerous changes | USPSTF recommends cervical screening for women 21-65 with various test options |
| Skin checks | Clinical visual examination of skin for suspicious lesions | USPSTF: insufficient evidence for routine screening; dermatology groups suggest targeted approaches |
| Ovarian screening | CA-125 blood test or transvaginal ultrasound | USPSTF recommends AGAINST screening average-risk women (no mortality benefit, significant harms) |
| Lung (LDCT) | Low-dose CT scan for high-risk individuals | USPSTF recommends for adults 50-80 with significant smoking history |
*These are general guidelines for average-risk populations. Individual recommendations may differ based on personal and family history. Always refer clients to their healthcare provider.
Why screening is complicated¶
Screening sounds like a no-brainer: find cancer early, treat it early, save lives. But the reality is more complex.
Benefits of screening:
- Can detect cancer at earlier, more treatable stages
- May reduce cancer mortality for certain cancers
- Provides peace of mind for many people
Potential harms:
- False positives: Lead to anxiety, additional testing, and sometimes invasive procedures for conditions that turn out not to be cancer
- Overdiagnosis: Detection of cancers that would never have caused symptoms or death (particularly relevant for prostate and some breast cancers)
- Procedure risks: Colonoscopy carries small but real risks; biopsies can cause complications
- Psychological impact: Living with a cancer diagnosis, even a slow-growing one, affects quality of life
This is why screening recommendations can be complex, and why shared decision-making between patients and physicians is so important. If keeping track of all the pros and cons feels like a lot, that's normal—you don't need to be the screening expert; you just need to support your clients as they talk things through with their doctor.
Your role in screening conversations¶
When clients ask about screening, your job is to:
-
Encourage discussion with their physician: "That's a great question to bring to your doctor at your next visit."
-
Support informed decision-making: "Screening is something where the right answer can be different for different people. Your doctor can help you think through the benefits and risks based on your specific situation."
-
Help with implementation: If a client's doctor has recommended a screening, you can help them schedule it, manage anxiety around it, and follow through.
-
Never recommend specific tests: Even if you think someone "obviously" needs a screening, that's a medical decision.
What About Advanced Screening?
Some longevity-focused clients may ask about emerging screening technologies they've heard about on podcasts or in online communities:
Multi-Cancer Early Detection Tests (like Galleri): These blood tests aim to detect multiple cancers from a single blood draw. Current evidence shows:
- Very high specificity (~99%). Few false positives
- Moderate overall sensitivity (~50%), meaning they miss about half of cancers
- Particularly low sensitivity for early-stage cancers (~17-27% for stage I)
- No evidence yet that they reduce mortality
- Large randomized trials are ongoingWhole-Body MRI: Some wellness centers offer full-body MRI scans. The evidence is concerning:
- Very high rate of incidental findings (up to 95% show something)
- ~30% require follow-up testing
- Only ~1-2% of findings are confirmed cancers
- Major radiology organizations recommend against it for average-risk individuals
- Significant cost ($1,000-$2,500+) typically not covered by insuranceThe coaching response: "Those are emerging technologies that some people find interesting. The evidence is still being gathered on whether they improve outcomes. If you're curious about them, it's worth discussing with your doctor, who can help you think through whether they make sense for your specific situation and risk level."
Key point: These technologies should complement, never replace, guideline-recommended screenings that have proven mortality benefits.
[CHONK: Genetics and Cancer Risk]
When genetics matter¶
Some clients have significant family histories of cancer or may already know they carry genetic variants that increase their risk. This affects their screening recommendations and risk management in ways that require physician and genetic counselor guidance.
What you should know¶
A small but meaningful percentage of cancers are driven primarily by inherited genetic variants:
BRCA1/BRCA2 (Hereditary Breast and Ovarian Cancer Syndrome)
- Carriers have lifetime breast cancer risk of approximately 65-79%
- Ovarian cancer risk: ~36-53% for BRCA1; ~11-25% for BRCA2
- Occurs in approximately 1 in 500 people in the general population; 1 in 40 in Ashkenazi Jewish populations
- Carriers typically receive enhanced screening (MRI plus mammography) and may consider risk-reducing surgery
Lynch Syndrome (Hereditary Nonpolyposis Colorectal Cancer)
- Lifetime colorectal cancer risk up to 52-82%
- Endometrial cancer risk: 40-60% in women
- Accounts for approximately 2-3% of all colorectal cancers
- Carriers typically receive more frequent colonoscopies (every 1-2 years)
What clients may ask:
- "Should I get genetic testing?"
- "Does my family history mean I'm at higher risk?"
- "My mom had cancer at 45. Should I be screened earlier?"
Your role with genetic questions¶
These are referral questions. Every time.
Genetic counselors and physicians specializing in cancer genetics are trained to:
- Evaluate family history patterns
- Determine if genetic testing is appropriate
- Interpret test results
- Recommend tailored screening and prevention strategies
Your job is to recognize when these conversations need to happen and facilitate the referral:
"Given your family history, this is really something to discuss with your doctor. They may suggest you meet with a genetic counselor who can help you understand your personal risk and what options might be available. Would it help to think through how to bring this up at your next appointment?"
Helping clients think about family history¶
You can appropriately ask about family history to understand context, but interpretation belongs to healthcare providers.
Red flags that suggest a client should discuss genetic counseling with their doctor:
- Multiple close relatives with the same cancer
- Cancer diagnosed at unusually young ages (before 50)
- Relatives with rare cancers
- Known genetic mutations in the family
- Ancestry associated with founder mutations (e.g., Ashkenazi Jewish heritage for BRCA)
Resource for clients:
For clients interested in learning more about genetics and health, Precision Nutrition has developed a thorough e-book on genetic testing that provides balanced, evidence-based information: Precision Nutrition's Genetic Testing E-Book.
[CHONK: Coaching Cancer Prevention]
Practical skills for cancer-related conversations¶
Cancer conversations require a special blend of empathy, accurate information, and clear boundaries. Here are practical approaches for common scenarios.
Managing cancer anxiety¶
Some clients carry significant anxiety about cancer, whether due to family history, health-related anxiety in general, or previous scares. Your job is to be a calming, grounded presence. Do not dismiss their concerns, but do not amplify them either.
Acknowledge without amplifying:
Client: "I'm constantly worried about getting cancer. My grandmother died of it, and I feel like it's just a matter of time."
Coach: "I can hear that this weighs on you. That's understandable given what you've seen in your family. Can I share what the research actually shows about what's in your control? Because the picture is more empowering than it might feel right now."
Ground in evidence:
When anxiety is high, concrete facts can be anchoring:
- "The research shows that 30-50% of cancers are linked to modifiable factors, meaning a significant portion of risk is things you can influence."
- "The lifestyle work you're doing—staying active, maintaining a healthy weight, eating well—this IS cancer prevention work."
Refer when appropriate:
Health anxiety that significantly impacts quality of life may warrant referral to a mental health professional. If a client is:
- Unable to stop thinking about cancer
- Avoiding activities due to cancer fears
- Experiencing panic or severe distress around the topic
...gently suggest they discuss these feelings with a counselor or therapist.
Supporting clients with family history¶
Clients with strong family histories of cancer need:
1. Validation: Their concerns are legitimate, not irrational
2. Empowerment: There are still things they can control
3. Appropriate referral: Their screening and prevention may need to be different
"Your family history is worth taking seriously, and I'm glad you're thinking about it. It means you might benefit from talking to your doctor about whether genetic counseling or a different screening schedule makes sense for you. In the meantime, the lifestyle factors we're working on. Those matter for everyone, including people with family history. We're not powerless here."
Clients with personal cancer history¶
If you work with cancer survivors, additional sensitivity is needed:
- Don't assume they want to talk about it: Let them lead.
- Recognize the complexity: They may have treatment-related side effects, fears of recurrence, or complicated feelings about their bodies.
- Focus on their current goals: Unless they bring up cancer, focus on what they came to coaching for.
- Know your limits: Cancer survivorship involves medical complexity. Collaborate with their oncology team; don't freelance.
Coaching in practice: Handling "should I be worried?" questions¶
The scenario: A client brings up a vague symptom and directly asks whether they should worry about cancer.
Client: "I've been having some digestive issues lately. Should I be worried about cancer?"
What NOT to do:
❌ Try to reassure or diagnose: "I'm sure it's nothing," or "That does sound concerning."
Why this doesn't work: You're not qualified to evaluate symptoms, and guessing (in either direction) can increase anxiety or delay needed care. It also steps well outside your scope of practice.
What TO do:
✅ Treat this as a referral moment and help them prepare for a medical conversation.
Coach: "I'm not able to evaluate symptoms like that. That's really something for your doctor. Have you mentioned this to them?"
If they haven't:
Coach: "I'd encourage you to bring this up. Digestive issues can have all kinds of causes, and your doctor can help figure out what's going on. Would it help to think through what you want to tell them?"
Key takeaways:
- You don't reassure or alarm
- You don't recommend specific tests
- You don't dismiss their concern
- You consistently facilitate the healthcare conversation
Coaching in practice: The fundamentals-first conversation¶
The scenario: A client feels overwhelmed by all the things they hear "cause cancer" and wonders how they can possibly avoid every risk.
Client: "I keep reading about all these things that cause cancer. It feels overwhelming. How can I possibly avoid it all?"
What NOT to do:
❌ Add to the overwhelm by listing every possible carcinogen or giving them a long list of advanced "biohacks" to chase.
Why this doesn't work: It reinforces a sense that everything is dangerous and can leave clients frozen, anxious, or focused on minor details instead of the big levers.
What TO do:
✅ Normalize their feelings and gently redirect their attention to the handful of fundamentals that account for most modifiable risk.
Coach: "I hear you, it can feel like everything is dangerous when you start reading about cancer risk. Here's what helps me think about it: there are a handful of factors that account for the vast majority of modifiable risk. Smoking, alcohol, body composition, physical activity, and basic nutrition patterns. Those are the big ones."
Coach: "The good news is you don't need to be perfect at everything. You don't need to eliminate every theoretical risk. You need to be reasonably consistent with the fundamentals. And honestly? The fundamentals are the same things we'd focus on for energy, for mood, for metabolic health, for feeling good. It's not a separate 'cancer prevention protocol.'"
Coach: "What we're already working on together? That IS cancer risk reduction, even if we don't talk about it that way."
Key takeaway: When clients feel overwhelmed, help them zoom out and focus on consistent fundamentals rather than chasing every possible risk.
Scope-safe language patterns summary¶
| Instead of... | Try... |
|---|---|
| "You should get screened for..." | "That's something to discuss with your doctor" |
| "This symptom might mean..." | "Any symptoms like that are worth mentioning to your doctor" |
| "Don't worry, you probably don't have cancer" | "I can't evaluate that, but your doctor can help you understand what's going on" |
| "You need to do X to prevent cancer" | "Research shows that X is associated with lower cancer risk" |
| "Your family history means you'll probably..." | "Your family history is worth discussing with your doctor or a genetic counselor" |
Deep Health integration¶
Cancer risk—and cancer conversations—touch multiple Deep Health dimensions:
Physical: The primary domain for this chapter. Body composition, exercise, nutrition, and metabolic health all directly influence cancer risk through biological pathways. The fundamentals deliver the greatest impact.
Emotional: Cancer is an emotionally loaded topic. Clients may carry fear, grief, or anxiety related to cancer, their own experiences or those of loved ones. Creating space for these emotions while remaining grounded and helpful is essential coaching work.
Mental: Understanding risk versus certainty is cognitively challenging. Helping clients think clearly about probabilistic information, "reducing risk is not eliminating risk," supports their mental well-being and decision-making.
Existential: Cancer often prompts reflection on mortality, meaning, and what matters. These conversations, when they arise, deserve presence and respect. You don't need to have answers; you need to be a thoughtful witness.
Relational: Cancer affects families. Clients may be navigating conversations with relatives about screening, genetic testing, or lifestyle changes. Supporting these relational dynamics can be part of your work.
Environmental: Carcinogen exposure in the environment (workplace, products, pollution) is real but largely outside coaching scope. If clients have specific environmental concerns, those warrant physician discussion.
[CHONK: Study guide questions]
Study guide questions¶
Here are some questions that can help you think through the material and prepare for the chapter exam. They're optional, but we recommend you try answering at least a few as part of your active learning process.
-
Why is "empowering, not fear-inducing" the right frame for cancer conversations? How does this affect your language choices?
-
Approximately what percentage of cancers are linked to modifiable lifestyle factors? What are the top factors?
-
How does insulin resistance connect to cancer risk? How does this relate to your Unit 2 learning?
-
A client asks you which cancer screening tests they should get. What is the appropriate response, and why?
-
What family history patterns might suggest a client should discuss genetic counseling with their doctor?
-
How would you explain to a client that "reducing risk is not eliminating risk" while still being encouraging?
Self-reflection questions:
-
Are you current on your age-appropriate cancer screenings? If not, what's stopping you from scheduling them?
-
Looking at the modifiable risk factors for cancer (body composition, alcohol, processed meat, physical activity, etc.), which one applies most to you, and what's one small change you could make?
Chapter exam¶
Open-book exam. Select the best answer for each question.
1. According to major research organizations, approximately what percentage of cancer cases are linked to modifiable lifestyle factors?
a) 5-10%
b) 15-20%
c) 30-50%
d) 70-80%
2. The International Agency for Research on Cancer (IARC) classifies alcohol as:
a) Group 2B: possibly carcinogenic
b) Group 2A: probably carcinogenic
c) Group 1: carcinogenic to humans
d) Not classified as a carcinogen
3. Which cancer sites are most strongly linked to excess body fat?
a) Lung and melanoma
b) Endometrial, kidney, liver, and colorectal
c) Prostate and bladder
d) Brain and bone
4. Physical activity reduces cancer risk through which mechanisms?
a) Improved insulin sensitivity and reduced inflammation
b) Enhanced immune function
c) Reduced circulating sex hormones
d) All of the above
5. Regarding cancer screening, the appropriate role for a health coach is to:
a) Recommend specific tests based on client age and risk factors
b) Interpret screening results and explain what they mean
c) Encourage discussion with healthcare providers and support implementation of their recommendations
d) Advise clients to skip screenings that have controversy around them
6. The phrase "reducing risk, not eliminating risk" is important because:
a) It helps manage expectations. Lifestyle changes lower probability but don't guarantee prevention
b) It gives coaches legal protection
c) It discourages clients from trying to change behaviors
d) It suggests lifestyle changes don't really matter
7. Insulin resistance increases cancer risk primarily through:
a) Direct damage to DNA
b) Activation of growth pathways (PI3K/Akt/mTOR) and increased IGF-1 availability
c) Reduced immune function
d) Increased vitamin deficiencies
8. When a client asks about genetic cancer risk based on their family history, the appropriate response is:
a) Assess their family tree and explain their genetic risk
b) Recommend specific genetic tests they should get
c) Refer them to discuss with their doctor or a genetic counselor
d) Tell them not to worry because genetics are only a small factor
9. Lynch syndrome primarily increases risk for which cancers?
a) Breast and ovarian
b) Colorectal and endometrial
c) Lung and melanoma
d) Prostate and bladder
10. A client says, "I've been having some unusual symptoms. Could this be cancer?" The appropriate response is:
a) "Let me assess your symptoms and tell you what I think"
b) "Don't worry, I'm sure it's nothing serious"
c) "That sounds concerning. You should get that checked immediately"
d) "I'm not able to evaluate symptoms. That's something to discuss with your doctor. Have you mentioned this to them?"
11. What is the current scientific consensus on alcohol and cancer risk?
a) Moderate drinking is protective against cancer
b) Only heavy drinking increases cancer risk
c) There is no safe level of alcohol consumption for cancer risk
d) Red wine is protective while other alcohol increases risk
12. Advanced screening technologies like multi-cancer early detection (MCED) tests currently:
a) Are proven to reduce cancer mortality
b) Have very high sensitivity, catching nearly all cancers
c) Have high specificity but moderate sensitivity, particularly low for early-stage cancers
d) Are recommended by USPSTF for all adults
13. Visceral fat increases cancer risk through:
a) Chronic inflammation and inflammatory cytokines
b) Hyperinsulinemia and growth factor activation
c) Adipokine imbalance (increased leptin, decreased adiponectin)
d) All of the above
14. The most appropriate way to frame cancer risk conversations is:
a) Focus on all the things that could go wrong to motivate behavior change
b) Emphasize what clients CAN control while acknowledging uncertainty
c) Avoid the topic entirely to prevent anxiety
d) Guarantee that lifestyle changes will prevent cancer
15. When a client with a family history of breast cancer asks about their risk, you should:
a) Explain BRCA genetics and calculate their likely risk percentage
b) Recommend they get genetic testing
c) Validate their concern and encourage discussion with their doctor about whether genetic counseling is appropriate
d) Tell them family history doesn't matter as much as lifestyle
Works cited¶
References¶
-
World Health Organization. Preventing cancer. WHO Activities; unknown. https://www.who.int/activities/preventing-cancer
-
American Cancer Society. New study finds 40% of cancer cases and almost half of all deaths in the U.S. linked to modifiable risk factors. 2024. https://pressroom.cancer.org/releases?item=1341
-
GBD 2019 Cancer Risk Factors Collaborators. The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet; 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9395583/
-
Zhang Y, Pan X, Chen J, Cao A, Zhang Y, Xia L, et al. Combined lifestyle factors, incident cancer, and cancer mortality: a systematic review and meta-analysis of prospective cohort studies. British Journal of Cancer. 2020;122(7):1085-1093. doi:10.1038/s41416-020-0741-x
-
WHO Regional Office for Europe. No level of alcohol consumption is safe for our health. 2022. https://www.who.int/europe/news-room/04-01-2023-no-level-of-alcohol-consumption-is-safe-for-our-health
-
Rumgay H, Shield K, Charvat H, Ferrari P, Sornpaisarn B, Obot I, et al. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. The Lancet Oncology. 2021;22(8):1071-1080. doi:10.1016/s1470-2045(21)00279-5
-
Jun S, Park H, Kim U, Choi EJ, Lee HA, Park B, et al. Cancer risk based on alcohol consumption levels: a comprehensive systematic review and meta-analysis. Epidemiology and Health. 2023;45:e2023092. doi:10.4178/epih.e2023092
-
Jun S et al.. Alcoholic beverage consumption and female breast cancer risk: A systematic review and meta-analysis. Alcohol Clin Exp Res; 2024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11629438/
-
Centers for Disease Control and Prevention. Obesity and Cancer. 2025. https://www.cdc.gov/cancer/risk-factors/obesity.html
-
Shi X, Deng G, Wen H, Lin A, Wang H, Zhu L, et al. Role of body mass index and weight change in the risk of cancer: A systematic review and meta-analysis of 66 cohort studies. Journal of Global Health. 2024;14. doi:10.7189/jogh.14.04067
-
Wilson RB, Lathigara D, Kaushal D. Systematic Review and Meta-Analysis of the Impact of Bariatric Surgery on Future Cancer Risk. International Journal of Molecular Sciences. 2023;24(7):6192. doi:10.3390/ijms24076192
-
Diao X, Ling Y, Zeng Y, Wu Y, Guo C, Jin Y, et al. Physical activity and cancer risk: a dose‐response analysis for the Global Burden of Disease Study 2019. Cancer Communications. 2023;43(11):1229-1243. doi:10.1002/cac2.12488
-
Yang L, Courneya KS, Friedenreich CM. The Physical Activity and Cancer Control (PACC) framework: update on the evidence, guidelines, and future research priorities. British Journal of Cancer. 2024;131(6):957-969. doi:10.1038/s41416-024-02748-x
-
Hermelink R, Leitzmann MF, Markozannes G, Tsilidis K, Pukrop T, Berger F, et al. Sedentary behavior and cancer–an umbrella review and meta-analysis. European Journal of Epidemiology. 2022;37(5):447-460. doi:10.1007/s10654-022-00873-6
-
Szablewski L. Insulin Resistance: The Increased Risk of Cancers. Current Oncology. 2024;31(2):998-1027. doi:10.3390/curroncol31020075
-
Clarke CS et al.. Associations between glycemic traits and colorectal cancer: a Mendelian randomization analysis. J Natl Cancer Inst; 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9086764/
-
Akkız H, Şimşek H, Balcı D, Ülger Y, Onan E, Akçaer N, et al. Inflammation and cancer: molecular mechanisms and clinical consequences. Frontiers in Oncology. 2025;15. doi:10.3389/fonc.2025.1564572
-
U.S. Preventive Services Task Force*. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine. 2009;151(10):716-726. doi:10.7326/0003-4819-151-10-200911170-00008
-
U.S. Preventive Services Task Force. Colorectal Cancer: Screening. 2021. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening
-
U.S. Preventive Services Task Force*. Screening for Prostate Cancer: U.S. Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine. 2008;149(3):185-191. doi:10.7326/0003-4819-149-3-200808050-00008
-
Hoffman RM, Wolf AMD, Raoof S, Guerra CE, Church TR, Elkin EB, et al. Multicancer early detection testing: Guidance for primary care discussions with patients. Cancer. 2025;131(7). doi:10.1002/cncr.35823
-
American College of Radiology. ACR Statement on Screening Total Body MRI. 2023. https://www.acr.org/News-and-Publications/Media-Center/2023/ACR-Statement-on-Screening-Total-Body-MRI
-
ACOG Committee. Hereditary Cancer Syndromes and Risk Assessment. 2019. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2019/12/hereditary-cancer-syndromes-and-risk-assessment
-
PDQ Cancer Genetics Editorial Board. Genetics of Breast and Gynecologic Cancers (PDQ)–Health Professional Version. National Cancer Institute; 2025. https://www.ncbi.nlm.nih.gov/books/NBK65767/
-
PDQ Cancer Genetics Editorial Board. Genetics of Colorectal Cancer (PDQ)–Health Professional Version. National Cancer Institute; 2025. https://www.ncbi.nlm.nih.gov/books/NBK126744/
-
Park J, Karnati H, Rustgi SD, Hur C, Kong X, Kastrinos F. Impact of population screening for Lynch syndrome insights from the All of Us data. Nature Communications. 2025;16(1). doi:10.1038/s41467-024-52562-5
-
Brown KA, Scherer PE. Update on Adipose Tissue and Cancer. Endocrine Reviews. 2023;44(6):961-974. doi:10.1210/endrev/bnad015
-
Harborg S, Larsen HB, Elsgaard S, Borgquist S. Metabolic syndrome is associated with breast cancer mortality: A systematic review and meta‐analysis. Journal of Internal Medicine. 2025;297(3):262-275. doi:10.1111/joim.20052