Unit 3: Advanced Topics & Disease Prevention¶
Chapter 3.17: Metabolic Disease & Inflammation¶
[CHONK: 1-minute summary]
What you'll learn in this chapter:
- How insulin resistance develops and progresses toward Type 2 Diabetes
- The concept of "inflammaging": chronic low-grade inflammation that accelerates aging
- What inflammation biomarkers like hsCRP measure (and what coaches can/cannot do with this information)
- Evidence that metabolic disease can be reversed through lifestyle changes
- How to support clients with metabolic risk factors within your scope of practice
- When metabolic concerns require medical referral
The big idea: Metabolic disease—particularly insulin resistance and Type 2 Diabetes—and chronic inflammation aren't separate problems. They're deeply interconnected, and both accelerate aging. The hopeful news: research shows these conditions can often be improved or even reversed through lifestyle changes. But here's where it gets tricky for coaches: metabolic disease sits squarely at the intersection of coaching and medicine. Understanding the biology helps you support clients effectively. But understanding your scope boundaries keeps them safe. This chapter gives you both.
What this means for your clients: Many of your clients either have metabolic concerns already (perhaps their doctor mentioned "prediabetes") or they're at risk. With this chapter, you'll understand what's happening in their bodies, know the evidence for improvement, and be able to support their lifestyle changes while staying firmly within your scope, always working alongside, never in place of, their medical team.
Introduction¶
In Chapter 2.8, we covered metabolic health strategies that benefit everyone: blood sugar management, meal composition, and time-restricted eating. That chapter was about optimization for healthy people.
This chapter is different. Here, we're going deeper into what happens when metabolic health breaks down: when insulin resistance develops, when Type 2 Diabetes emerges, when chronic inflammation accelerates aging. We're talking about disease processes, not just optimization.
Why does this matter for longevity coaches?
Metabolic dysfunction is one of the biggest threats to healthspan and lifespan. Metabolic syndrome is a cluster of conditions including high blood sugar, high blood pressure, excess abdominal fat, and abnormal cholesterol, and it affects roughly one in three American adults.28 Having metabolic syndrome increases the risk of dying from heart disease by 44 percent and from diabetes by more than five-fold.28
And chronic inflammation? It's been called "inflammaging", a persistent, low-grade inflammatory state that accelerates aging and contributes to virtually every age-related disease.40
If those numbers feel a little alarming, that's a normal reaction. You don't need to memorize the exact percentages; just remember that metabolic health and inflammation are major levers you and your clients can influence.
But here's the hopeful part: both metabolic disease and chronic inflammation respond to lifestyle changes. The DiRECT trial showed that 46 percent of people with Type 2 Diabetes achieved remission at one year through an intensive diet program.24 Regular exercise reduces inflammatory markers significantly.48
As a coach, you won't diagnose these conditions, interpret labs, or prescribe treatments. Your medical colleagues do that. But you will help clients implement the lifestyle changes their doctors recommend. You'll support behavior change, build sustainable habits, and help clients navigate the emotional complexity of living with metabolic concerns.
That's why you need to understand this biology. Not to practice medicine, but to be an effective partner in care.
Let's start by understanding what we're dealing with.
[CHONK: Metabolic Health: The Foundation]
Metabolic Health: The Foundation¶
Before we talk about metabolic disease, let's establish what metabolic health actually means.
What Is Metabolic Health?¶
Metabolic health refers to how well your body processes and uses energy from food. When you eat, your body breaks down carbohydrates into glucose (blood sugar), which cells use for fuel. The hormone insulin, produced by your pancreas, acts like a key that allows glucose to enter cells.
In a metabolically healthy person, this system works smoothly:
- Blood sugar rises after eating, then returns to baseline
- Insulin does its job efficiently
- Cells readily absorb glucose for energy
- The body can switch easily between burning glucose and burning fat (this is called metabolic flexibility)
You covered metabolic flexibility in detail in Chapter 2.8. The key point: healthy metabolic function means your body can adapt to different energy demands and fuel sources without getting stuck.
The Five Markers of Metabolic Syndrome¶
Doctors identify metabolic syndrome when someone has three or more of five specific conditions:20
- Large waist circumference: More than 40 inches for men, more than 35 inches for women (these thresholds vary by ethnicity)
- High triglycerides: 150 mg/dL or higher
- Low HDL cholesterol: Less than 40 mg/dL for men, less than 50 mg/dL for women
- High blood pressure: 130/85 mmHg or higher
- High fasting blood sugar: 100 mg/dL or higher
Important scope note: These are medical diagnostic criteria. You cannot diagnose metabolic syndrome. Only a licensed healthcare provider can do that. But understanding these markers helps you appreciate what your clients are dealing with when their doctor identifies metabolic concerns.
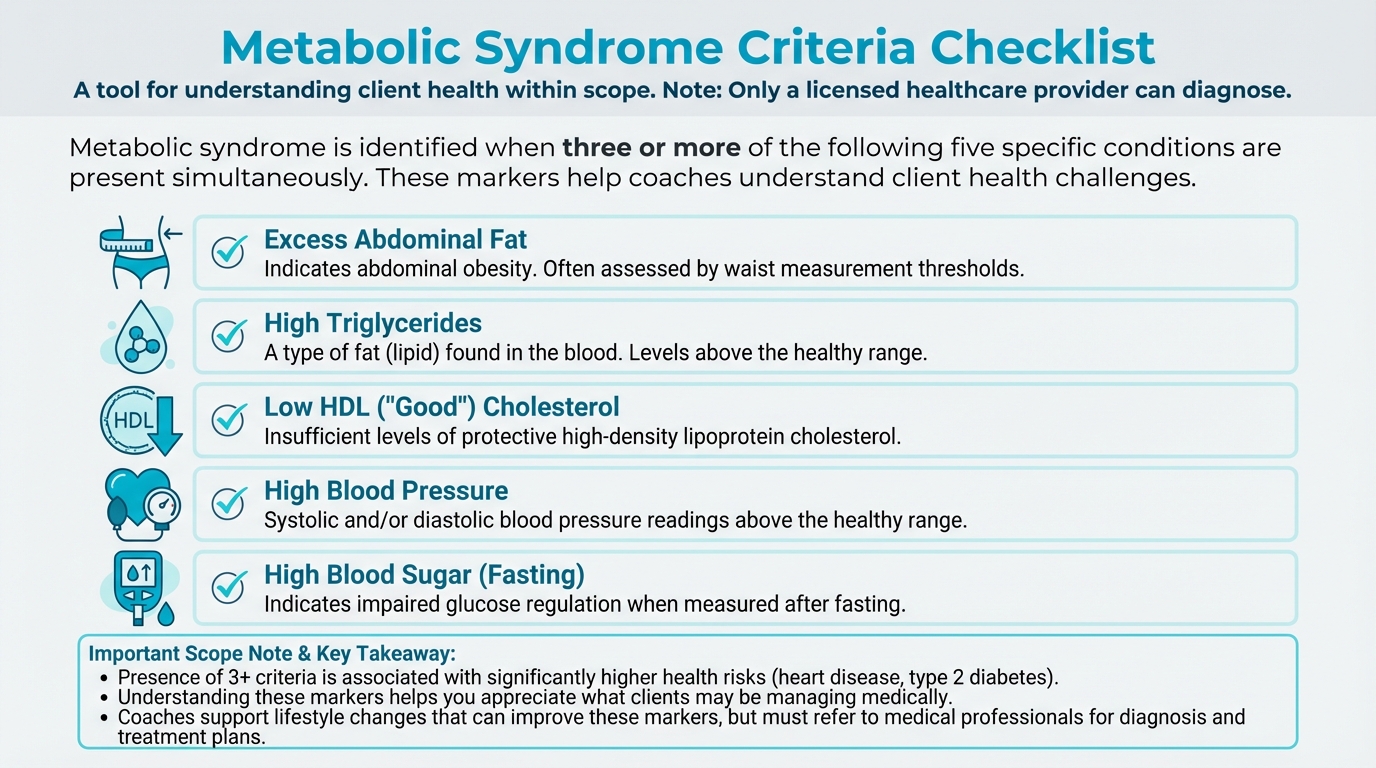
Figure: 5 criteria visual
The Metabolic Health Continuum¶
Here's a helpful way to think about metabolic health: it exists on a continuum.
Optimal metabolic health → Suboptimal → Metabolic syndrome → Prediabetes → Type 2 Diabetes
This isn't a sudden cliff; it's a gradual slope. People don't wake up one day with Type 2 Diabetes; they slide there over years, often decades.
Research from the Whitehall II study showed that glycemia (blood sugar levels) rise slowly for about 10 years before diabetes diagnosis, then accelerate rapidly in the final two to five years before diagnosis.47
If the idea of a decade-long slide toward diabetes feels daunting, that's understandable. The upside is that this long lead-in creates many chances to help clients change course. (That's actually good news.)
What this means: there's often a long window for intervention. Lifestyle changes can slow or stop the slide, sometimes even reverse it.
Why This Matters for Longevity¶
The mortality statistics are sobering. Metabolic syndrome is associated with:
- 24 percent higher all-cause mortality
- 44 percent higher heart disease mortality
- More than five-fold higher diabetes-related mortality.28
But the flip side is equally important: improving metabolic health reduces these risks. In the Look AHEAD trial, participants who achieved even temporary diabetes remission had 40 percent fewer cardiovascular events and 33 percent fewer cases of chronic kidney disease compared to those who never achieved remission.19
This is why metabolic health is central to longevity coaching. It's modifiable. It's high-impact. And coaches can make a real difference through behavior change support.
[CHONK: Insulin Resistance: The Slow Slide]
Insulin Resistance: The Slow Slide¶
Insulin resistance is often the first step on the path to Type 2 Diabetes. Understanding how it develops helps you appreciate why the lifestyle interventions you'll support actually work.
How Insulin Normally Works¶
Let's start with normal function. When you eat carbohydrates:
- Your digestive system breaks them down into glucose
- Glucose enters your bloodstream
- Your pancreas detects rising blood sugar and releases insulin
- Insulin travels through the blood and "knocks on the doors" of cells (technically, insulin binds to receptors on cell surfaces)
- Cells "open the door" and let glucose in
- Cells use glucose for energy
- Blood sugar returns to normal levels
Think of insulin as a key that lets glucose into cells. In a healthy system, the key works smoothly, and glucose flows from the bloodstream into cells efficiently.
What Happens When Cells Become Resistant¶
Insulin resistance means the cells stop responding well to insulin's signal. The key is in the lock, but the door doesn't open as easily.
Here's what happens at the cellular level:
When cells are constantly exposed to high insulin levels (often due to frequent eating, high-sugar diets, or excess body fat), they start "turning down the volume" on their insulin receptors. It's like living next to a loud highway. Eventually, you stop hearing it.9
Several factors contribute to this resistance:
Excess fat, especially visceral fat. Fat cells aren't just storage containers. They're metabolically active, releasing hormones and inflammatory signals. Excess fat, particularly the fat stored around organs (visceral fat), releases inflammatory molecules like TNF-α and interleukins that interfere with insulin signaling.27
Ectopic fat accumulation. "Ectopic" means "in the wrong place." When fat accumulates in the liver and muscles, places it shouldn't be stored, it disrupts how these tissues respond to insulin. The liver becomes less able to suppress glucose production; muscles become less able to absorb glucose.54
Chronic inflammation. Inflammatory molecules directly interfere with the insulin signaling pathway. We'll explore this more in the inflammaging section, but the key point is: inflammation and insulin resistance fuel each other.2
Mitochondrial dysfunction. Mitochondria are tiny structures inside cells that produce energy (think of them as cellular power plants). When they don't work well, often due to inactivity, excess nutrients, or aging, cells become less efficient at processing glucose.56
The Compensation Phase¶
Here's where the body tries to fight back.
When cells become resistant to insulin, the pancreas responds by producing more insulin. If the key doesn't work as well, make more keys. This is called compensatory hyperinsulinemia.
For a while, this works. Blood sugar stays normal because there's enough extra insulin to overcome the resistance. This is why insulin resistance often exists for years before blood sugar rises enough to be detected on standard tests.
But this compensation comes at a cost. Chronically high insulin levels have their own problems. They promote fat storage, inflammation, and may even worsen insulin resistance over time (Lewis et al., 2023).
The Progression to Type 2 Diabetes¶
Eventually, the pancreas can't keep up.
The beta cells in the pancreas, the cells that produce insulin, become exhausted. By the time someone develops impaired glucose tolerance (a stage between normal and diabetes), they've already lost 60 to 85 percent of their insulin-secreting capacity.15
The timeline varies, but research suggests:
- Slow glycemic rise for roughly 10 years
- Rapid deterioration in the final two to five years before diagnosis
- Beta cell function declining steeply in the final five years47
If that timeline feels intimidating, keep in mind that it also means there is usually plenty of time for clients and their medical teams to intervene. You don't need to diagnose where someone is on this curve to help them start shifting their habits.
Once both insulin resistance AND inadequate insulin production are present, Type 2 Diabetes develops.37
Early Warning Signs¶
Insulin resistance doesn't announce itself with obvious symptoms. But there are patterns clients (and their doctors) might notice:
- Increased hunger, especially shortly after eating
- Fatigue, especially after high-carbohydrate meals
- Difficulty losing weight, particularly around the abdomen
- Skin changes like dark, velvety patches in body folds (called acanthosis nigricans)
- Polycystic ovary syndrome (PCOS) in women, which is strongly linked to insulin resistance
Scope reminder: If a client describes these patterns, you can acknowledge that these symptoms are worth discussing with their doctor. You cannot tell them they have insulin resistance. That's a medical determination.
The Reversibility Window¶
Here's the hopeful part: insulin resistance is not a one-way street.
The same lifestyle factors that cause insulin resistance can reverse it, at least in the early stages. Weight loss, exercise, and dietary changes can restore insulin sensitivity. The earlier someone intervenes, the better their chances of preventing progression to diabetes.
Research shows that combined aerobic and resistance training reduced fasting insulin and HOMA-IR (a measure of insulin resistance) substantially in sedentary adults.44 Low-glycemic diets—those that don't spike blood sugar rapidly—also improve insulin sensitivity.55
The key message for clients: metabolic health problems develop gradually, which means there's usually time to make changes. And those changes work—which is exactly where your coaching skills can make a difference.
Coaching in practice: Explaining insulin resistance to clients¶
The scenario: A client tells you their doctor mentioned "insulin resistance," and they look worried. They say, "I have no idea what that actually means, but it sounds bad."
What NOT to do:
- Launch into a long, technical lecture about receptors, mitochondria, and inflammatory molecules.
Why it doesn't work: Clients usually don't need the molecular details, and too much jargon can make them feel overwhelmed or ashamed.
What TO do:
Offer a simple, visual explanation and connect it directly to what they can do.
Sample dialogue:
Client: "My doctor said I'm insulin resistant. I don't really get what that means."
Coach: "It can definitely sound scary. Want a simple way to picture it?"
Client: "Yes, please."
Coach: "Think of insulin as a delivery person bringing packages (glucose) to your cells. When you're metabolically healthy, cells open the door right away. The delivery is efficient. With insulin resistance, cells stop opening the door as quickly. The body responds by sending more delivery people. For a while, packages still get delivered. But eventually, packages pile up in the bloodstream. That's high blood sugar. The good news? Regular movement and dietary changes are like training your cells to open the door again. They become more responsive, and the system works better."
Client: "So exercise and changing how I eat actually help my cells listen better?"
Coach: "Exactly. Exercise helps your cells become more sensitive to insulin again, and the types of foods you eat affect how much your blood sugar spikes. Over time, those changes often help people's metabolic markers improve. Your doctor can tell you what's happening with your numbers."
Key phrases that stay in scope:
- "Exercise helps your cells become more sensitive to insulin again."
- "The types of foods you eat affect how much your blood sugar spikes."
- "These changes often help people's metabolic markers improve. Your doctor can tell you what's happening with your numbers."
Phrases to avoid (out of scope):
- "Your insulin resistance is mild/moderate/severe."
- "Based on what you've told me, you probably have prediabetes."
- "You should take metformin."
[CHONK: Inflammaging: The Fire Within]
Inflammaging: The Fire Within¶
Now let's talk about inflammation, specifically, the kind of chronic, low-grade inflammation that increases with age and accelerates aging processes.
Acute vs. Chronic Inflammation¶
First, some context. Inflammation isn't inherently bad.
Acute inflammation is your body's healthy response to injury or infection. Cut your finger, and the area becomes red, warm, and swollen. That's inflammation at work, bringing immune cells to fight infection and repair tissue. This kind of inflammation is temporary, targeted, and essential for survival.
Chronic inflammation is different. It's a persistent, low-level inflammatory state that doesn't resolve. Instead of a fire that burns hot and then goes out, think of smoldering embers that never fully extinguish. This kind of inflammation damages tissues over time and contributes to virtually every age-related disease.40
What Is Inflammaging?¶
The term "inflammaging" combines "inflammation" and "aging." It describes the chronic, progressive, low-grade systemic inflammatory state that develops as people get older.3
Key features of inflammaging:
- It's chronic: always present, not triggered by acute infection or injury
- It's low-grade: not enough to cause obvious symptoms, but enough to cause damage over time
- It's systemic: affecting the whole body, not just one location
- It's progressive: tends to worsen with age unless actively addressed
Inflammaging has been linked to frailty, disability, cognitive decline, cardiovascular disease, Type 2 Diabetes, neurodegeneration, and mortality.50
The Mechanisms Behind Inflammaging¶
Several interconnected processes drive inflammaging:
Cellular senescence and SASP. As cells age, some enter a state called senescence. They stop dividing but don't die. These "zombie cells" release inflammatory molecules (collectively called the Senescence-Associated Secretory Phenotype, or SASP). The more senescent cells accumulate, the more inflammation they produce.4
Mitochondrial dysfunction. Remember those cellular power plants? When mitochondria malfunction, they produce reactive oxygen species (ROS), unstable molecules that damage cells and trigger inflammatory pathways.56
Gut microbiome changes. As people age, their gut bacteria change. There is typically less diversity and more pro-inflammatory species. The gut barrier can become more permeable—sometimes called "leaky gut"—allowing bacterial products to enter the bloodstream and trigger inflammation.7
Immune system changes (immunosenescence). The immune system becomes less efficient with age, but paradoxically more prone to producing inflammatory signals. It's like a security system that's constantly setting off false alarms while missing actual threats.50
NF-κB and inflammasome activation. These are molecular pathways that, when chronically activated, drive sustained inflammation. Various age-related stressors—damaged DNA, misfolded proteins, mitochondrial dysfunction—can trigger these pathways.29
If all these pathways and acronyms feel like alphabet soup, that's OK. You don't need to memorize each mechanism; what's important is recognizing that many age-related processes nudge the body toward a chronic, simmering inflammatory state.
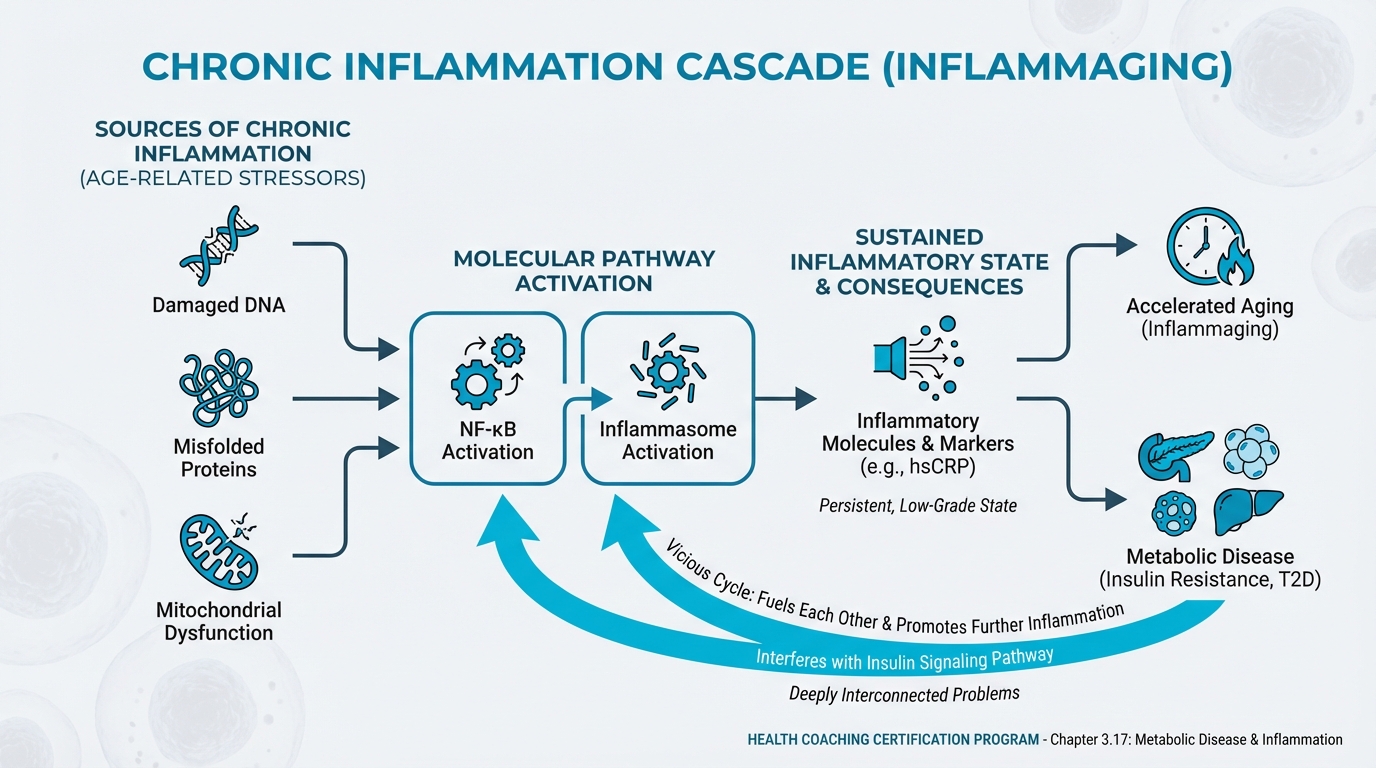
Figure: Chronic inflammation pathways
Inflammation Biomarkers¶
Doctors can measure inflammation through blood tests. The most common is hsCRP (high-sensitivity C-reactive protein), a protein the liver produces in response to inflammation, measured in milligrams per liter (mg/L).
General hsCRP ranges (for educational purposes only):
- Less than 1.0 mg/L: lower cardiovascular risk
- 1.0-3.0 mg/L: moderate risk
- Greater than 3.0 mg/L: higher risk.39
Critical scope reminder: You cannot interpret a client's hsCRP results. You cannot tell them their inflammation is "high" or "low." If a client shows you their test results, you can explain what hsCRP measures in general terms, but interpretation belongs to their physician.
Other inflammation-related markers doctors may assess include ESR (erythrocyte sedimentation rate), IL-6 (interleukin-6), and TNF-α (tumor necrosis factor alpha). Again, interpretation is medical scope.
What the Research Shows About hsCRP and Mortality¶
The research connecting inflammation to mortality is sobering:
- In the UK Biobank study (more than 400,000 people), those in the highest CRP quartile had 68 percent higher risk of premature death compared to the lowest quartile.31
- In a Shanghai cohort, CRP above 3 mg/L was associated with 53 percent higher all-cause mortality and 71 percent higher cardiovascular mortality compared to CRP under 1 mg/L.23
- A composite inflammaging score predicted mortality (41 percent higher risk per standard deviation increase) independent of epigenetic aging measures.12
- ESR between 20-50 mm/hr predicted 23 percent higher mortality compared to ESR under 20; ESR above 50 predicted 89 percent higher mortality.16
These statistics underscore why reducing chronic inflammation matters for longevity.
If all of those risk percentages are starting to blur together, you're not alone. The key takeaway is simple: higher levels of chronic inflammation consistently track with higher risk of disease and early death.
Sources of Chronic Inflammation¶
Inflammaging isn't just about aging. Lifestyle factors play a major role:
Diet. Western dietary patterns—high in processed foods, refined sugars, and saturated fats—activate inflammatory pathways. These foods increase gut permeability, alter the microbiome, and directly trigger inflammatory signaling.33
Obesity, especially visceral fat. Fat tissue actively produces inflammatory molecules. The more excess fat (particularly abdominal fat), the more inflammation.41
Sedentary behavior. Physical inactivity increases inflammatory markers. Conversely, regular exercise is one of the most powerful anti-inflammatory interventions available.22
Chronic stress. Sustained psychological stress activates the HPA axis and sympathetic nervous system, shifting immune function toward pro-inflammatory states. Stress hormones activate inflammatory pathways including NF-κB.32
Poor sleep. Sleep deprivation increases inflammatory markers. This connects to your learning from the sleep chapters. Sleep isn't just about energy; it's about inflammation control.
Smoking. Smokers show higher CRP, IL-6, and other inflammatory markers. Even after quitting, some elevation may persist.14
Gut dysbiosis. Imbalanced gut bacteria can increase intestinal permeability, allowing bacterial products (particularly lipopolysaccharides, or LPS) to enter circulation and trigger systemic inflammation.8
What Coaches Can Do¶
Here's where your role becomes clear. You cannot diagnose inflammation or interpret test results. But you can:
- Educate clients about inflammation as a modifiable factor in aging
- Support behavior changes that reduce inflammation (movement, dietary quality, sleep, stress management)
- Encourage clients to discuss inflammation concerns with their medical providers
- Help clients implement anti-inflammatory recommendations from their healthcare team
[CHONK: Lifestyle Reversal: It's Not Too Late]
Lifestyle Reversal: It's Not Too Late¶
If metabolic disease and inflammation sound like inevitable consequences of aging, here's the hopeful counter-narrative: substantial evidence shows these conditions can be improved, and sometimes reversed, through lifestyle changes.
The DiRECT Trial: A Landmark Study¶
The Diabetes Remission Clinical Trial (DiRECT) changed how we think about Type 2 Diabetes. Researchers enrolled people with Type 2 Diabetes (diagnosed within the previous six years) and put the intervention group through an intensive diet program using total diet replacement (very low calorie).
Results:
- 46 percent achieved remission at one year (intervention) vs. 4 percent (control).24
- 36-40 percent remained in remission at two years.52,11
- 13 percent were still in remission at five years.13
The dose-response relationship with weight loss was striking. At one year:
- Less than 5 kg lost: 7 percent remission
- 5-10 kg lost: 34 percent remission
- 10-15 kg lost: 57 percent remission
- 15+ kg lost: 86 percent remission.24
If all those percentages are starting to blur together, that's completely fine. The key idea is that greater, sustained weight loss generally means a higher chance of remission, especially earlier in the disease process.
What "remission" means: HbA1c under 6.5 percent (or fasting glucose under 126 mg/dL) without diabetes medications for at least two months. Remission doesn't mean "cured." The underlying susceptibility remains, and weight regain typically brings blood sugar back up.
The Mechanisms of Reversal¶
Research has clarified why weight loss reverses Type 2 Diabetes:
Liver fat reduction. After just one week of very low calorie diet, fasting glucose normalized and hepatic (liver) insulin sensitivity improved. The liver was releasing less glucose into the bloodstream.30
Pancreatic fat reduction. Pancreatic fat dropped from about 8 percent to 6.2 percent after eight weeks, and first-phase insulin secretion more than doubled.30 The pancreas was recovering function.
Restored beta cell function. The insulin-producing cells, previously overwhelmed, began functioning better as the metabolic stress lifted.46
The key insight: Type 2 Diabetes isn't a fixed state. In many cases, it reflects overwhelmed metabolic machinery that can recover when the burden is lightened.
Beyond DiRECT: What Works for Metabolic Improvement¶
While DiRECT used intensive total diet replacement, other interventions also improve metabolic health:
Exercise, especially combined training. A meta-analysis found combined aerobic and resistance training reduced fasting insulin by about 1.0 standard deviation and HOMA-IR (insulin resistance measure) by about 0.95 standard deviations in sedentary adults.44 That's a meaningful improvement.
The ACSM consensus statement notes that moderate-intensity aerobic training lowers HbA1c by approximately 0.5-0.7 percent in people with Type 2 Diabetes.1
Diet + exercise outperforms diet alone. A randomized trial showed that adding exercise to a weight-loss diet produced about twice the improvement in whole-body insulin sensitivity compared to diet alone, at the same amount of weight loss.6 Exercise provides benefits beyond just what the scale shows.
Dietary patterns matter. Low-glycemic index diets (those that don't spike blood sugar rapidly) significantly improve insulin resistance compared to high-glycemic diets.55 Mediterranean-style diets, rich in vegetables, olive oil, and fish, improve multiple metabolic markers and reduce Type 2 Diabetes risk.38
Time-restricted eating. As you learned in Chapter 2.8, TRE can improve glucose homeostasis. Research in animals shows TRE can restore the daily oscillations in respiratory exchange ratio (a measure of fuel switching) even without weight loss.53 Fasting periods longer than 12 hours shift metabolism toward fat burning and may trigger beneficial cellular cleanup processes like autophagy.35
Gut health interventions. Meta-analyses show probiotics and prebiotics produce modest but significant improvements in glycemic markers in people with Type 2 Diabetes, including reductions in HbA1c, fasting glucose, and HOMA-IR.49
Anti-Inflammatory Lifestyle Interventions¶
For reducing chronic inflammation, the evidence points to:
Exercise, the most consistent evidence. A meta-analysis of aerobic exercise in older adults found significant reductions in CRP (about 0.85 mg/L), IL-6, and TNF-α, along with increases in anti-inflammatory IL-10.48 Lifelong exercisers have lower baseline inflammatory markers than sedentary peers.42
Mediterranean dietary patterns. A 2025 meta-analysis of randomized trials found that Mediterranean diets significantly improved hsCRP, IL-6, and IL-17.36 The pattern matters more than any single food.
Mind-body practices. Meta-analyses show yoga, meditation, and Tai Chi decrease pro-inflammatory cytokines.34,25
Weight loss. Reducing excess body fat, especially visceral fat, reduces the inflammatory signals emanating from adipose tissue.
Complications Reduction in Look AHEAD¶
The Look AHEAD trial followed over 5,000 people with Type 2 Diabetes through an intensive lifestyle intervention focused on weight loss. While the trial didn't show a significant reduction in cardiovascular events overall, secondary analyses revealed important findings:
- Participants who achieved any remission had 40 percent fewer cardiovascular events (HR 0.60).
- They also had 33 percent fewer cases of chronic kidney disease (HR 0.67).19
Even short-term remission conferred benefit. This underscores that metabolic improvement, even if not permanent, matters for long-term outcomes.
If those outcomes make you worry that you have to produce "trial-level" results with every client, take a breath. You're not trying to recreate a research study; you're helping real people make meaningful, sustainable changes in the context of their actual lives. (That's enough.)
Setting Realistic Expectations¶
While the evidence for lifestyle reversal is strong, it's important to be realistic with clients:
Durability requires maintenance. In DiRECT, among those in remission at two years, only about 26 percent remained in remission at five years.18 Weight regain typically leads to blood sugar returning to diabetic levels.
Not everyone responds equally. Longer diabetes duration and greater loss of beta cell function predict lower likelihood of remission.17 Earlier intervention works better.
Lifestyle changes require support. The intensive support in DiRECT and Look AHEAD contributed to outcomes. Real-world implementation without that support may show smaller effects.
If that sounds a bit discouraging, remember that even temporary improvements in blood sugar and weight can reduce complications and buy people more healthy years. Progress still counts, even if remission isn't permanent.
This is where you come in. Your role as a coach, helping clients maintain changes over time, is exactly what's needed to translate trial results into real-world impact.
If this feels like a lot of responsibility, that's normal. Your job isn't to guarantee remission; it's to help clients make sustainable changes that move them in a better direction over time.
Coaching in practice: The hierarchy of metabolic interventions¶
The scenario: A client with newly diagnosed prediabetes says, "Just tell me which supplements and gadgets I need to fix this," but they're sleeping five hours a night, barely moving, and eating most meals from a drive-thru.
What NOT to do:
- Start with third-tier "biohacks" like supplements while ignoring foundations.
- Overwhelm them with a dozen simultaneous changes.
Why it doesn't work: This majors in the minors and often leaves clients frustrated when the basics would have had the biggest impact.
What TO do:
Lay out a clear hierarchy so you focus first on what moves the needle most.
First tier, strongest evidence:
- Weight management (if excess weight is present): remission rates directly correlate with weight loss.
- Regular movement. Both aerobic and resistance training improve insulin sensitivity.
- Dietary pattern quality: less processed food, more vegetables, appropriate portions.
Second tier. Supportive evidence:
- Meal timing and composition (post-meal walks, protein/fiber first, time-restricted eating).
- Sleep optimization. Poor sleep worsens insulin resistance.
- Stress management. Chronic stress elevates blood sugar and inflammation.
Third tier. Emerging/modest evidence:
- Specific gut health interventions (fermented foods, fiber diversity).
- Anti-inflammatory foods (beyond general dietary quality).
Critical reminder: You support these interventions through behavior change coaching. The medical team monitors results, adjusts medications, and determines whether metabolic goals are being met.
[CHONK: Coaching Metabolic Health (Within Scope)]
Coaching Metabolic Health Within Scope¶
Now let's get practical. How do you support clients with metabolic concerns while staying firmly within your scope of practice?
If you ever feel a bit anxious about overstepping, that's actually a good sign—it means you're paying attention to your professional boundaries.
What Coaches CAN Do¶
Educate about metabolic health. You can explain what insulin resistance is, how blood sugar works, what inflammation means. The educational content in this chapter helps clients understand why lifestyle changes matter.
Support lifestyle change implementation. This is your core function. When a client's doctor says "you need to lose weight" or "increase your activity," you help make that happen. Goal-setting, habit formation, barrier troubleshooting, accountability. These are coaching skills that translate directly to metabolic health improvement. (This is where coaches really shine.)
Encourage and support medical recommendations. If a physician prescribes metformin, you can help the client remember to take it and manage side effects through their medical team. If a dietitian creates a meal plan, you can help them follow it consistently.
Facilitate behavior change conversations. Use motivational interviewing to help clients explore their own motivations for change. "What matters most to you about improving your metabolic health?" "What would be different in your life if your blood sugar were better controlled?"
Help clients prepare for medical appointments. You can help clients write down questions, track their habits (so they can report accurately to their doctor), and process information from appointments.
Coordinate with the medical team (with consent). With client permission, you can communicate with physicians, share observations about client progress, and ensure everyone is on the same page.
What Coaches CANNOT Do¶
Diagnose metabolic conditions. If a client says "I think I have insulin resistance," you cannot confirm or deny. Your response: "That's worth discussing with your doctor. They can run the appropriate tests."
Interpret lab results. If a client shows you their glucose, HbA1c, or triglyceride results, you cannot tell them if their numbers are "good" or "bad." You can explain in general terms what these tests measure, but interpretation is medical scope. "Your doctor is the best person to tell you what these results mean for you specifically."
Recommend supplements for metabolic conditions. You cannot tell a client to take berberine, chromium, cinnamon, or any other supplement for blood sugar management. Even natural supplements can interact with medications and affect metabolic function.
A special note on berberine: This supplement has significant research showing glucose-lowering effects similar to diabetes medications. Fasting glucose reductions of about 0.5-0.8 mmol/L and HbA1c reductions of about 0.4-0.7 percent across meta-analyses.51,10 Because of this medication-like effect, berberine is firmly in medical scope. If clients ask about it, your response: "Berberine has research behind it, but because it affects blood sugar similarly to some medications, it's something to discuss with your doctor, especially if you're on any medications."
Recommend medication changes. You cannot suggest clients start, stop, or change diabetes medications. Even "you should talk to your doctor about reducing your medication," while well-intentioned, crosses into medical decision-making.
Provide medical nutrition therapy. Individualized meal planning for metabolic disease management requires a registered dietitian. You can support general healthy eating patterns and help clients follow dietitian-created plans, but creating therapeutic diets is outside coaching scope.
Supporting Clients WITH Type 2 Diabetes¶
Many of your clients will already have a Type 2 Diabetes diagnosis. You're not treating their diabetes. Their medical team does that. But you can provide valuable support:
Help them implement lifestyle changes their medical team recommends. Most diabetes treatment plans include lifestyle components. You're the person who helps make those happen.
Support medication adherence. If remembering medications is challenging, you can help with systems and accountability, always in support of, not instead of, their medical plan.
Address the emotional component. A diabetes diagnosis can bring shame, fear, and denial. You can provide a supportive space to process these feelings (while referring to mental health professionals if distress is significant).
Celebrate progress. When their doctor reports improved HbA1c, acknowledge the behavior changes that contributed. "Your consistency with those post-dinner walks is really showing up."
Navigate setbacks without judgment. Blood sugar management has ups and downs. Help clients learn from setbacks rather than spiraling into self-criticism.
When to Refer¶
Some situations require immediate medical referral:
Red flags that require urgent physician contact:
- Symptoms of very high blood sugar (extreme thirst, frequent urination, blurred vision, unexplained weight loss)
- Symptoms of very low blood sugar (shakiness, confusion, sweating, rapid heartbeat), especially if client is on glucose-lowering medication
- Signs of diabetic ketoacidosis (fruity breath, nausea/vomiting, confusion, abdominal pain)
- Non-healing wounds or sores, especially on feet
- Sudden vision changes
- Chest pain, shortness of breath, or other cardiovascular symptoms
Situations requiring physician follow-up:
- Client hasn't seen their doctor about metabolic concerns in the past year
- Client reports significant changes in their condition
- Client wants to change their medication or supplement regimen
- Client's lifestyle changes are producing rapid improvements (medication may need adjustment to prevent low blood sugar)
- Client expresses interest in pursuing diabetes remission
CGM in Coaching: A Special Consideration¶
Continuous glucose monitors (CGMs) are increasingly available over-the-counter, and some non-diabetic clients use them for optimization purposes. If a client uses a CGM, scope considerations apply:
What you can do:
- Help them notice patterns (e.g., "what do you observe about your glucose after different types of meals?")
- Support behavior experiments they design (e.g., "let's see what happens when you take a walk after dinner")
- Provide education about normal glucose variation in healthy people
What you cannot do:
- Interpret whether their glucose patterns indicate pathology
- Diagnose insulin resistance or prediabetes based on CGM data
- Make supplement or medication recommendations based on glucose data
Important context: Healthy adults on CGM typically spend about 96 percent of time in the 70-140 mg/dL range, with about 1 percent of time briefly below 70 mg/dL. These brief dips are often clinically insignificant.43,45 Overmonitoring can cause unnecessary anxiety. Some research on wearable health devices shows a subset of users develop monitoring-related anxiety, a phenomenon called "orthosomnia" for sleep trackers.5,21
If a client seems anxious about their CGM data, that's worth addressing. (And if you've ever felt this way looking at your own wearable data, you're in good company.) Data should empower, not stress.
Professional Language¶
The words you choose matter. Here's how to discuss metabolic topics appropriately:
Instead of: "Your blood sugar is too high."
Say: "How did your doctor explain your blood sugar results?"
Instead of: "You have insulin resistance."
Say: "It sounds like your doctor mentioned some metabolic concerns. What did they recommend?"
Instead of: "You should take chromium for blood sugar."
Say: "Any supplements that affect blood sugar are worth discussing with your doctor first."
Instead of: "Based on what you've told me, I think you're prediabetic."
Say: "Those symptoms are worth mentioning to your doctor. They can run tests to see what's going on."
Instead of: "You're doing great. Your inflammation is probably down."
Say: "You've been really consistent with these changes. Your doctor can check how your markers are responding at your next visit."
Coaching in practice: 'I think I have diabetes'¶
The scenario: A client tells you, "I think I have diabetes. I'm always tired after meals."
What NOT to do:
- "Yes, that sounds like diabetes. You probably have blood sugar issues." (This is diagnosing.)
- "You should cut all carbs." (This is prescriptive nutrition.)
- "Take some berberine. It helps with blood sugar." (This is supplement recommendation for a medical condition.)
What TO do:
Validate their concern, encourage medical evaluation, and shift into pattern exploration—without giving a diagnosis.
Sample dialogue:
Client: "I think I have diabetes. I'm always tired after meals."
Coach: "Feeling wiped out after you eat can definitely be frustrating. It's also something your doctor will want to know about, because they can run tests to see what's going on."
Client: "So you think I have diabetes?"
Coach: "I can't say what is or isn't going on—that's your doctor's role. What I can do is help you notice patterns so you have good information to share. For example, have you noticed whether certain meals make you more tired than others?"
Client: "Yeah, big pasta lunches seem to knock me out."
Coach: "That's really useful to know. Let's track that for a bit so you and your doctor have clearer data to work with, and we can experiment with meals that leave you feeling more steady."
Why this stays in scope:
- Doesn't diagnose
- Encourages medical evaluation
- Offers coaching support (pattern exploration) that stays in scope
[CHONK: Deep Health Integration]
Deep Health Integration¶
Metabolic health and inflammation touch all six dimensions of Deep Health. Let's map the connections:
Physical¶
This is the primary dimension: metabolic function is a physical process. Insulin sensitivity, glucose regulation, and inflammation all manifest in the body. The physical dimension includes:
- Body composition (muscle mass, fat distribution)
- Cardiovascular function (metabolic disease increases CVD risk)
- Energy levels (metabolic dysfunction often causes fatigue)
- Sleep quality (poor sleep worsens insulin resistance; poor metabolic health worsens sleep)
Mental¶
Blood sugar fluctuations affect cognitive function. Research shows:
- High glucose variability is associated with worse cognitive performance
- Both hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) can cause mental fog
- Chronic inflammation is linked to cognitive decline and neurodegeneration
For your clients, this might manifest as difficulty concentrating, brain fog after meals, or mental fatigue. These are worth noting, and worth mentioning to their medical team. You don't need to have all the answers about why a client feels foggy; noticing patterns and encouraging follow-up is enough.
Emotional¶
Metabolic disease brings emotional complexity:
- Shame: Many people feel embarrassed about metabolic diagnoses, especially given societal stigma around weight
- Fear: Worries about disease progression, complications, becoming "diabetic"
- Denial: Some clients minimize the significance of metabolic concerns
- Frustration: Especially when lifestyle changes don't produce immediate results
- Food anxiety: Obsessive monitoring can lead to disordered relationships with food
Your role includes holding space for these emotions, normalizing them, and helping clients separate their identity from their metabolic status. If you're not always sure exactly what to say, that's OK; simply listening and validating can be extremely powerful.
Social¶
Social factors profoundly influence metabolic health:
- Food environment: Social eating patterns, family meals, workplace snacks
- Support systems: People with supportive families have better adherence to lifestyle changes
- Social determinants: Access to healthy food, safe places to exercise, healthcare
- Social comparison: Seeing others "eat whatever they want" while struggling with blood sugar
Social eating is particularly relevant. Help clients develop strategies for navigating social situations without feeling isolated or deprived.
Environmental¶
The built environment shapes metabolic health:
- Food environment: Proximity to grocery stores vs. fast food, food deserts
- Physical activity infrastructure: Walkability, parks, gym access
- Work environment: Desk jobs, shift work (which disrupts circadian rhythms and worsens metabolic health)
- Toxin exposure: Some environmental chemicals (endocrine disruptors) may contribute to metabolic dysfunction
As a coach, you can't change a client's environment single-handedly, but you can help them identify environmental barriers and brainstorm solutions.
Existential¶
Metabolic health connects to bigger-picture concerns:
- Longevity and mortality: Clients may confront their own mortality when diagnosed with metabolic disease
- Quality of life: Fear of complications—blindness, amputation, kidney failure—looms large
- Purpose and identity: "Am I going to be 'a diabetic' forever?"
- Future planning: Concerns about being healthy for children, grandchildren, retirement
These existential dimensions can be powerful motivators for change, or sources of overwhelming despair. Help clients connect their daily choices to their larger values and purposes.
You're not acting as a therapist here, but you can listen, reflect what you hear, and, when appropriate, suggest mental health support. (You don't have to carry this alone.)
[CHONK: Case Study]
Case Study: Marcus¶
Client Profile:
Marcus, 54, was recently told by his doctor that he has "prediabetes" with an HbA1c of 6.1 percent. His doctor also mentioned his hsCRP was "a little elevated" at 2.8 mg/L. Marcus was given a pamphlet about diet and exercise and told to come back in six months. He found a longevity coach (you) because he doesn't want to "become diabetic like my father." (Understandably.)
What Marcus shares:
- Works long hours at a desk job
- Eats most meals on the go or at restaurants
- Hasn't exercised regularly in years
- Sleeps about 5-6 hours per night
- Drinks alcohol socially, 2-3 nights per week
- Feels "constantly stressed" about work
- Waist circumference: 42 inches
- Gets winded climbing stairs
Initial Coach Response:
You recognize several factors that contribute to metabolic dysfunction and inflammation: sedentary work, poor sleep, stress, possible excess visceral fat, and limited meal control. These are all coachable areas.
You also recognize your boundaries: you won't tell Marcus his numbers are "bad," diagnose insulin resistance, or prescribe a treatment plan. You'll support behavior change.
First Session Approach:
You start with values exploration: "What matters most to you about your health right now?"
Marcus talks about his father's diabetes complications (foot amputation) and wanting to be healthy for his kids. This is powerful motivation material.
You ask: "What did your doctor recommend? What do you think might be most helpful?"
Marcus admits the pamphlet felt generic. (We hear that a lot.) He knows he "should eat better and exercise more" but doesn't know where to start.
Collaborative Planning:
Rather than prescribing, you explore: "If you were going to make one change this week, what feels most doable?"
Marcus decides that eating breakfast at home instead of grabbing a muffin is something he could try.
You help make this specific: What breakfast? When? What needs to be in the house? What might get in the way?
Progress Over Time:
Over several months, Marcus:
- Adds a 15-minute post-dinner walk (building to 30 minutes)
- Shifts breakfast and lunch toward higher protein, more vegetables
- Starts strength training twice weekly with a trainer
- Prioritizes seven hours of sleep on weekdays
- Reduces alcohol to weekends only
Six-Month Follow-Up:
Marcus returns to his doctor. His HbA1c has dropped to 5.8 percent (no longer in prediabetes range), and his hsCRP is now 1.4 mg/L. He's lost 12 pounds, mostly from the midsection.
If these changes sound simple but powerful, that's the point—small, consistent shifts can add up.
What the Coach Did Well:
- Supported medical recommendations without overstepping
- Used client values as motivation anchor
- Started with small, achievable changes
- Built gradually toward full lifestyle improvement
- Celebrated process (behavior changes) not just outcomes (lab results)
- Never interpreted lab results. Let the doctor do that
- Connected Marcus with a trainer for the exercise component
What the Coach Didn't Do:
- Didn't diagnose or confirm prediabetes
- Didn't interpret lab values
- Didn't recommend supplements
- Didn't create a meal plan (helped with behavioral strategies instead)
- Didn't tell Marcus to stop his doctor-prescribed plan
[CHONK: Study guide questions]
Study Guide Questions¶
Here are some questions that can help you think through the material and prepare for the chapter exam. They're optional, but we recommend you try answering at least a few as part of your active learning process.
-
What is insulin resistance, and what are the key factors that contribute to its development?
-
What does "inflammaging" mean, and why is it relevant to longevity coaching?
-
What were the key findings of the DiRECT trial regarding Type 2 Diabetes remission?
-
A client shows you their blood work and asks "Is my A1C good?" How do you respond while staying in scope?
-
What are three lifestyle interventions with strong evidence for improving metabolic health?
-
Why might a supplement like berberine be outside coaching scope to recommend?
-
How does chronic inflammation connect to metabolic dysfunction?
-
What red flags in a client with metabolic concerns should prompt immediate medical referral?
Self-reflection questions:
-
Pay attention to your energy after meals this week. Do you crash 2-3 hours after eating certain foods? What patterns do you notice?
-
What's your waist circumference? This simple measurement is a better indicator of metabolic health than scale weight alone.
Chapter Exam¶
1. Insulin resistance is best described as:
a) When the pancreas stops producing insulin
b) When cells become less responsive to insulin's signal
c) When blood sugar drops too low
d) When the immune system attacks insulin-producing cells
2. True or False: Health coaches can interpret a client's HbA1c results and tell them if the number is "good" or "bad."
3. In the DiRECT trial, what percentage of participants achieved diabetes remission at one year?
a) 14%
b) 28%
c) 46%
d) 68%
4. Which of the following CAN a health coach appropriately do?
a) Diagnose prediabetes based on symptoms the client describes
b) Recommend berberine supplementation for blood sugar support
c) Help a client implement the lifestyle changes their doctor recommended
d) Interpret inflammation markers from blood tests
5. Inflammaging refers to:
a) Acute inflammation from injury
b) Chronic, low-grade inflammation that increases with age
c) High fever during infection
d) Allergic inflammation
6. True or False: A client's ability to switch between burning glucose and fat for fuel is called metabolic flexibility.
7. Which lifestyle intervention has the MOST consistent evidence for reducing inflammatory markers in older adults?
a) Supplement stacks
b) Sauna protocols
c) Regular exercise
d) Intermittent fasting
8. A client says "I think I have diabetes." The appropriate coaching response is:
a) "Yes, based on your symptoms, that's likely."
b) "Let's check your blood sugar right now."
c) "That's worth discussing with your doctor. They can run the appropriate tests."
d) "You should start taking berberine."
9. True or False: According to Look AHEAD trial findings, participants who achieved any diabetes remission had 40% fewer cardiovascular events.
10. High-sensitivity C-reactive protein (hsCRP) is a marker of:
a) Kidney function
b) Liver enzymes
c) Systemic inflammation
d) Thyroid function
11. The compensation phase of insulin resistance refers to:
a) When cells start responding to insulin again
b) When the pancreas produces more insulin to overcome resistance
c) When blood sugar normalizes after meals
d) When fat is released from storage
12. True or False: Coaches cannot recommend supplements for metabolic conditions because supplements are always ineffective.
13. Which dietary pattern has the most evidence for reducing inflammation?
a) Carnivore diet
b) Mediterranean-style diet
c) Juice cleanse
d) High-protein, low-fat diet
14. When a client with Type 2 Diabetes shows rapid improvement from lifestyle changes, a coach should:
a) Congratulate them and continue as planned
b) Suggest they reduce their medications
c) Encourage them to follow up with their doctor, as medications may need adjustment
d) Tell them they're probably in remission
15. True or False: Visceral fat (fat stored around organs) is more metabolically problematic than subcutaneous fat (fat under the skin).
Works cited¶
References¶
-
ACSM. Exercise/Physical Activity in Individuals with Type 2 Diabetes: A Consensus Statement. Med Sci Sports Exerc; 2022. https://pmc.ncbi.nlm.nih.gov/articles/PMC8802999/
-
Ahn B. Advances in Insulin Resistance—Molecular Mechanisms, Therapeutic Targets, and Future Directions. International Journal of Molecular Sciences. 2025;26(6):2574. doi:10.3390/ijms26062574
-
Andonian BJ, Hippensteel JA, Abuabara K, Boyle EM, Colbert JF, Devinney MJ, et al. Inflammation and aging-related disease: A transdisciplinary inflammaging framework. GeroScience. 2024;47(1):515-542. doi:10.1007/s11357-024-01364-0
-
Baechle JJ, Chen N, Makhijani P, Winer S, Furman D, Winer DA. Chronic inflammation and the hallmarks of aging. Molecular Metabolism. 2023;74:101755. doi:10.1016/j.molmet.2023.101755
-
Baron KG, Abbott S, Jao N, Manalo N, Mullen R. Orthosomnia: Are Some Patients Taking the Quantified Self Too Far?. Journal of Clinical Sleep Medicine. 2017;13(02):351-354. doi:10.5664/jcsm.6472
-
Beals JW, Kayser BD, Smith GI, Schweitzer GG, Kirbach K, Kearney ML, et al. Dietary weight loss-induced improvements in metabolic function are enhanced by exercise in people with obesity and prediabetes. Nature Metabolism. 2023;5(7):1221-1235. doi:10.1038/s42255-023-00829-4
-
Caldarelli M, Rio P, Marrone A, Giambra V, Gasbarrini A, Gambassi G, et al. Inflammaging: The Next Challenge—Exploring the Role of Gut Microbiota, Environmental Factors, and Sex Differences. Biomedicines. 2024;12(8):1716. doi:10.3390/biomedicines12081716
-
Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, et al. Metabolic Endotoxemia Initiates Obesity and Insulin Resistance. Diabetes. 2007;56(7):1761-1772. doi:10.2337/db06-1491
-
Chandrasekaran P, Weiskirchen R. Cellular and Molecular Mechanisms of Insulin Resistance. Current Tissue Microenvironment Reports. 2024;5(3):79-90. doi:10.1007/s43152-024-00056-3
-
Cheung AWL, et al. Overall and Sex-Specific Effect of Berberine on Glycemic and Insulin-Related Traits: A Systematic Review and Meta-Analysis. J Nutr; 2023. https://pubmed.ncbi.nlm.nih.gov/37598753/
-
Corrao S, Falcone F, Mirarchi L, Amodeo S, Calvo L. Type 2 Diabetes Mellitus Remission, Dream or Reality? A Narrative Review of Current Evidence and Integrated Care Strategies. Diabetes Therapy. 2025;16(8):1557-1579. doi:10.1007/s13300-025-01761-4
-
Cribb L, Hodge AM, Yu C, Li SX, English DR, Makalic E, et al. Inflammation and Epigenetic Aging Are Largely Independent Markers of Biological Aging and Mortality. The Journals of Gerontology: Series A. 2022;77(12):2378-2386. doi:10.1093/gerona/glac147
-
Diabetes UK. Weight loss can put type 2 diabetes into remission for at least five years, DiRECT study reveals. Press release; 2024. https://www.diabetes.org.uk/about-us/news-and-views/weight-loss-can-put-type-2-diabetes-remission-least-five-years-reveal-latest-findings
-
Elisia I, Lam V, Cho B, Hay M, Li MY, Yeung M, et al. The effect of smoking on chronic inflammation, immune function and blood cell composition. Scientific Reports. 2020;10(1). doi:10.1038/s41598-020-76556-7
-
Feingold KR, et al. Pathogenesis of Type 2 Diabetes Mellitus. Endotext; 2024. https://www.ncbi.nlm.nih.gov/books/NBK279115/
-
Fest J, Ruiter R, Mooijaart S, Ikram MA, van Eijck CHJ, Stricker BH. Erythrocyte sedimentation rate as an independent prognostic marker for mortality: a prospective population‐based cohort study. Journal of Internal Medicine. 2018;285(3):341-348. doi:10.1111/joim.12853
-
Ghusn W, Hurtado MD, Acosta A. Weight-centric treatment of type 2 diabetes mellitus. Obesity Pillars. 2022;4:100045. doi:10.1016/j.obpill.2022.100045
-
Glasgow University. Diet intervention links longer remissions of type 2 diabetes and improved health over 5 years. Press release; 2024. https://www.gla.ac.uk/news/archiveofnews/2024/february/headline_1049216_en.html
-
Gregg EW, Chen H, Bancks MP, Manalac R, Maruthur N, Munshi M, et al. Impact of remission from type 2 diabetes on long-term health outcomes: findings from the Look AHEAD study. Diabetologia. 2024;67(3):459-469. doi:10.1007/s00125-023-06048-6
-
Hamooya BM, Siame L, Muchaili L, Masenga SK, Kirabo A. Metabolic syndrome: epidemiology, mechanisms, and current therapeutic approaches. Frontiers in Nutrition. 2025;12. doi:10.3389/fnut.2025.1661603
-
Jahrami H, Trabelsi K, Husain W, Ammar A, BaHammam AS, Pandi-Perumal SR, et al. Prevalence of Orthosomnia in a General Population Sample: A Cross-Sectional Study. Brain Sciences. 2024;14(11):1123. doi:10.3390/brainsci14111123
-
Karabetian A, et al. The impact of exercise on chronic systemic inflammation: a systematic review and meta–meta-analysis. Sport Sci Health; 2025. https://link.springer.com/article/10.1007/s11332-025-01445-3
-
Ke J, Liu Q, Liu X, Wu K, Qiu H, Song J, et al. Prognostic value of C-reactive protein predicting all-cause and cause-specific mortality: a prospective cohort study in Shanghai, China. BMJ Open. 2025;15(8):e101532. doi:10.1136/bmjopen-2025-101532
-
Lean ME, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. The Lancet. 2018;391(10120):541-551. doi:10.1016/S0140-6736(17)33102-1
-
Lee S, Tsai P, Yu K, Chan T. Effects of Mind–Body Interventions on Immune and Neuroendocrine Functions: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Healthcare. 2025;13(8):952. doi:10.3390/healthcare13080952
-
Greenway F, Loveridge B, Grimes RM, Tucker TR, Alexander M, Hepford SA, et al. Physiologic Insulin Resensitization as a Treatment Modality for Insulin Resistance Pathophysiology. International Journal of Molecular Sciences. 2022;23(3):1884. doi:10.3390/ijms23031884
-
Li M, Chi X, Wang Y, Setrerrahmane S, Xie W, Xu H. Trends in insulin resistance: insights into mechanisms and therapeutic strategy. Signal Transduction and Targeted Therapy. 2022;7(1). doi:10.1038/s41392-022-01073-0
-
Li W, Chen D, Peng Y, Lu Z, Kwan M, Tse LA. Association Between Metabolic Syndrome and Mortality: Prospective Cohort Study. JMIR Public Health and Surveillance. 2023;9:e44073. doi:10.2196/44073
-
Liang R, Qi X, Cai Q, Niu L, Huang X, Zhang D, et al. The role of NLRP3 inflammasome in aging and age-related diseases. Immunity & Ageing. 2024;21(1). doi:10.1186/s12979-023-00395-z
-
Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. 2011;54(10):2506-2514. doi:10.1007/s00125-011-2204-7
-
Liu S, Yang R, Zuo Y, Qiao C, Jiang W, Cheng W, et al. The association of circulating systemic inflammation with premature death and the protective role of the Mediterranean diet: a large prospective cohort study of UK biobank. BMC Public Health. 2024;24(1). doi:10.1186/s12889-024-18888-x
-
Liu Z, Lei M, Bai Y. Chronic Stress Mediates Inflammatory Cytokines Alterations and Its Role in Tumorigenesis. Journal of Inflammation Research. 2025;Volume 18:1067-1090. doi:10.2147/JIR.S485159
-
Margină D, Ungurianu A, Purdel C, Tsoukalas D, Sarandi E, Thanasoula M, et al. Chronic Inflammation in the Context of Everyday Life: Dietary Changes as Mitigating Factors. International Journal of Environmental Research and Public Health. 2020;17(11):4135. doi:10.3390/ijerph17114135
-
Mishra B, Agarwal A, George JA, Upadhyay AD, Nilima N, Mishra R, et al. Effectiveness of Yoga in Modulating Markers of Immunity and Inflammation: A Systematic Review and Meta-Analysis. Cureus. 2024. doi:10.7759/cureus.57541
-
Mishra S, Persons PA, Lorenzo AM, Chaliki SS, Bersoux S. Time-Restricted Eating and Its Metabolic Benefits. Journal of Clinical Medicine. 2023;12(22):7007. doi:10.3390/jcm12227007
-
Keshani M, Rafiee S, Heidari H, Rouhani MH, Sharma M, Bagherniya M. Mediterranean Diet Reduces Inflammation in Adults: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Nutrition Reviews. 2025. doi:10.1093/nutrit/nuaf213
-
NIDDK. Insulin Resistance & Prediabetes. National Institute of Diabetes and Digestive and Kidney Diseases; 2024. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance
-
Papadaki A, Nolen-Doerr E, Mantzoros CS. The Effect of the Mediterranean Diet on Metabolic Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults. Nutrients. 2020;12(11):3342. doi:10.3390/nu12113342
-
Reynolds HR. High-Sensitivity C-Reactive Protein and Cardiovascular Risk. UpToDate; 2024. https://www.uptodate.com/contents/c-reactive-protein-in-cardiovascular-disease
-
Saavedra D, Añé-Kourí AL, Barzilai N, Caruso C, Cho K, Fontana L, et al. Aging and chronic inflammation: highlights from a multidisciplinary workshop. Immunity & Ageing. 2023;20(1). doi:10.1186/s12979-023-00352-w
-
Savulescu-Fiedler I, Mihalcea R, Dragosloveanu S, Scheau C, Baz RO, Caruntu A, et al. The Interplay between Obesity and Inflammation. Life. 2024;14(7):856. doi:10.3390/life14070856
-
Schnohr A, et al. Does Lifelong Exercise Counteract Low-Grade Inflammation Associated with Aging?. Sports Med.; 2025. https://link.springer.com/article/10.1007/s40279-024-02152-8
-
Shah VN, DuBose SN, Li Z, Beck RW, Peters AL, Weinstock RS, et al. Continuous Glucose Monitoring Profiles in Healthy Nondiabetic Participants: A Multicenter Prospective Study. The Journal of Clinical Endocrinology & Metabolism. 2019;104(10):4356-4364. doi:10.1210/jc.2018-02763
-
Silva FM, Duarte-Mendes P, Teixeira AM, Soares CM, Ferreira JP. The effects of combined exercise training on glucose metabolism and inflammatory markers in sedentary adults: a systematic review and meta-analysis. Scientific Reports. 2024;14(1). doi:10.1038/s41598-024-51832-y
-
Sofizadeh S, Pehrsson A, Ólafsdóttir AF, Lind M. Evaluation of Reference Metrics for Continuous Glucose Monitoring in Persons Without Diabetes and Prediabetes. Journal of Diabetes Science and Technology. 2020;16(2):373-382. doi:10.1177/1932296820965599
-
Suleiman M, Marselli L, Cnop M, Eizirik DL, De Luca C, Femia FR, et al. The Role of Beta Cell Recovery in Type 2 Diabetes Remission. International Journal of Molecular Sciences. 2022;23(13):7435. doi:10.3390/ijms23137435
-
Tabák AG, Jokela M, Akbaraly TN, Brunner EJ, Kivimäki M, Witte DR. Trajectories of glycaemia, insulin sensitivity, and insulin secretion before diagnosis of type 2 diabetes: an analysis from the Whitehall II study. The Lancet. 2009;373(9682):2215-2221. doi:10.1016/S0140-6736(09)60619-X
-
Tayebi SM, Poorhabibi H, Heidary D, Amini MA, Sadeghi A. Impact of aerobic exercise on chronic inflammation in older adults: a systematic review and meta-analysis. BMC Sports Science, Medicine and Rehabilitation. 2025;17(1). doi:10.1186/s13102-025-01279-z
-
Paul P, Kaul R, Harfouche M, Arabi M, Al-Najjar Y, Sarkar A, et al. The effect of microbiome-modulating probiotics, prebiotics and synbiotics on glucose homeostasis in type 2 diabetes: A systematic review, meta-analysis, and meta-regression of clinical trials. Pharmacological Research. 2022;185:106520. doi:10.1016/j.phrs.2022.106520
-
Wrona MV, Ghosh R, Coll K, Chun C, Yousefzadeh MJ. The 3 I’s of immunity and aging: immunosenescence, inflammaging, and immune resilience. Frontiers in Aging. 2024;5. doi:10.3389/fragi.2024.1490302
-
Xie W, Su F, Wang G, Peng Z, Xu Y, Zhang Y, et al. Glucose-lowering effect of berberine on type 2 diabetes: A systematic review and meta-analysis. Frontiers in Pharmacology. 2022;13. doi:10.3389/fphar.2022.1015045
-
Xin Y, Davies A, Briggs A, McCombie L, Messow CM, Grieve E, et al. Type 2 diabetes remission: 2 year within-trial and lifetime-horizon cost-effectiveness of the Diabetes Remission Clinical Trial (DiRECT)/Counterweight-Plus weight management programme. Diabetologia. 2020;63(10):2112-2122. doi:10.1007/s00125-020-05224-2
-
Yan L, Rust BM, Palmer DG. Time-restricted feeding restores metabolic flexibility in adult mice with excess adiposity. Frontiers in Nutrition. 2024;11. doi:10.3389/fnut.2024.1340735
-
Yang Y, Wang T, Xie H, Hu PP, Li P. Experimental cell models of insulin resistance: overview and appraisal. Frontiers in Endocrinology. 2024;15. doi:10.3389/fendo.2024.1469565
-
Yu YT, et al. Dietary glycemic index and insulin resistance in non-diabetic adults. Front Nutr; 2025. https://pmc.ncbi.nlm.nih.gov/articles/PMC11864931/
-
Zuo L, Prather ER, Stetskiv M, Garrison DE, Meade JR, Peace TI, et al. Inflammaging and Oxidative Stress in Human Diseases: From Molecular Mechanisms to Novel Treatments. International Journal of Molecular Sciences. 2019;20(18):4472. doi:10.3390/ijms20184472