Unit 2: Core Interventions (The Protocol)¶
Chapter 2.7: Nutrition for Longevity¶
[CHONK: 1-minute summary]
What you'll learn in this chapter:
- How food affects aging biology through nutrient-sensing pathways (mTOR, AMPK, sirtuins)
- The Mediterranean and MIND dietary patterns. What they are and why they work
- Protein requirements for preventing muscle loss (sarcopenia) as we age
- Practical targets for fiber and vegetable intake
- Evidence-based guidance on what to limit (ultra-processed foods, alcohol)
- How to discuss nutrition within your coaching scope
- A sample day showing these principles in action
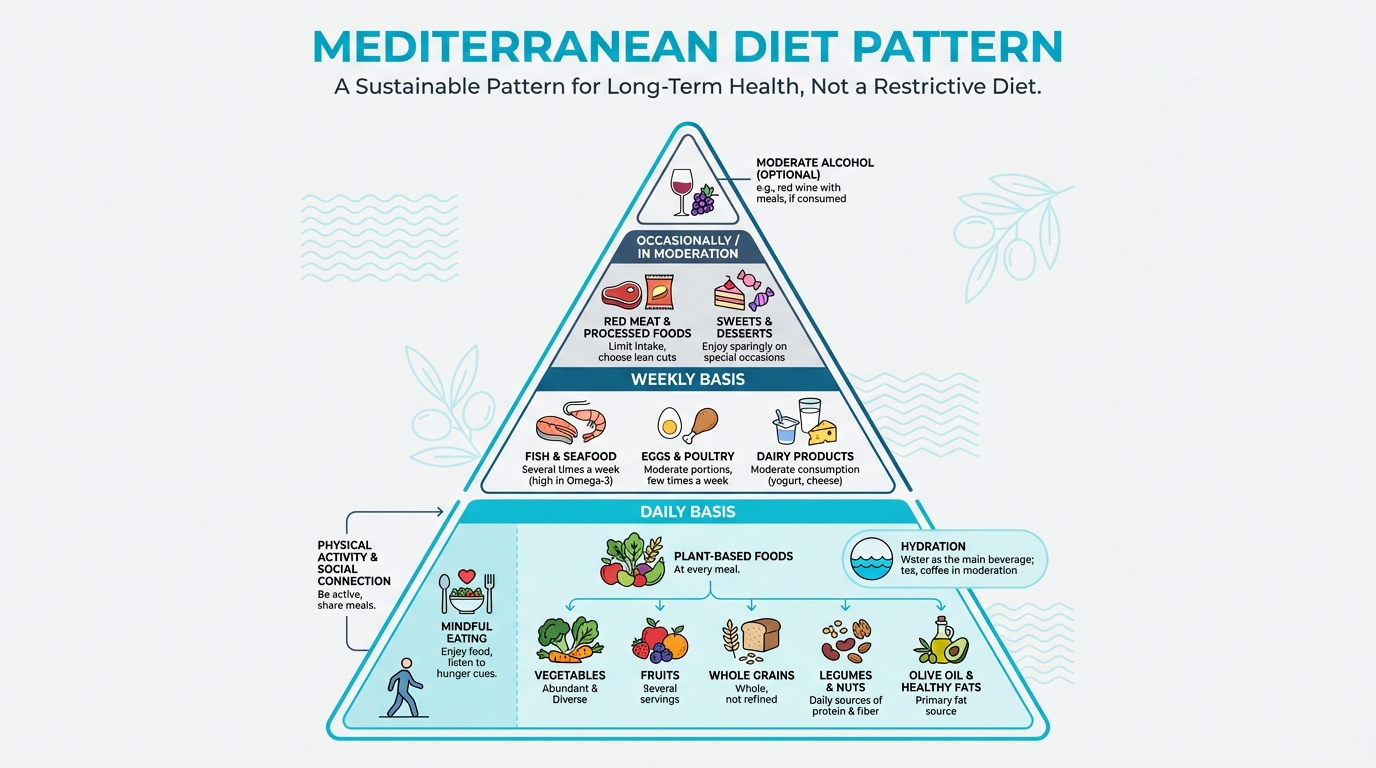
Figure: Visual representation of food groups, portions, frequencies
The big idea: Nutrition for longevity isn't about restriction or perfection. It's about consistently eating in ways that support your body's maintenance and repair systems. The research points clearly to a Mediterranean-style approach, adequate protein, abundant plants, and minimizing ultra-processed foods. This chapter gives you the evidence, the practical targets, and the coaching framework to help clients eat for a longer, healthier life.
[CHONK: Introduction: Why Nutrition for Longevity Is Different]
Introduction: More Than "Healthy Eating"¶
You probably already know that nutrition matters. But coaching nutrition for longevity is different from coaching for weight loss or performance. Here, we're playing a longer game, decades, not weeks.
When clients come to you wanting to "eat for longevity," they're asking a deeper question: How do I eat in a way that supports my body's ability to maintain itself, repair damage, and stay functional as I age?
That question connects directly to the biology you learned in Chapter 1.2. Remember the hallmarks of aging? Several of them—nutrient sensing, autophagy, mitochondrial function, inflammation—are directly influenced by what and how much you eat.
This isn't about finding the "perfect diet." It's about understanding which eating patterns consistently show up in longevity research, and helping clients build sustainable habits around those patterns.
What This Chapter Covers¶
We'll cover the what of eating for longevity:
- Which dietary patterns have the strongest evidence
- How much protein older adults need (it's more than you might think)
- Why fiber and plant diversity matter
- What to reduce and why
We won't cover when to eat. That's Chapter 2.8 (Metabolic Health & Nutrition Timing), where we'll discuss meal timing, time-restricted eating, and metabolic flexibility.
The Hierarchy: Essential → Valuable → Optional¶
Not all nutrition interventions are equal. Here's how to think about priorities:
Essential (focus here first):
- Adequate protein (prevents muscle loss)
- Abundant vegetables and fiber
- Minimizing ultra-processed foods
Valuable (add once essentials are solid):
- Mediterranean/MIND dietary pattern
- Omega-3 rich foods or supplementation
- Diverse plant foods for microbiome health
Optional (fine-tuning for those with fundamentals dialed):
- Specific supplements beyond basics
- Advanced meal composition strategies
- Precise macronutrient ratios
This hierarchy matters. Don't let clients obsess over omega-3 timing if they're eating processed food for most meals.
[CHONK: How Food Affects Aging Biology]
How Food Affects Aging Biology¶
Your cells have two basic modes: build mode and repair mode.
When you eat—especially protein—your cells shift into build mode. They focus on growth. When you haven't eaten for a while, your cells shift into repair mode. They focus on maintenance and cleanup.
Both modes are necessary: build mode maintains muscle, while repair mode cleans up cellular damage. The problem is when you're always in build mode—eating constantly, never giving your cells time to do maintenance.
Why This Matters for Longevity¶
As we age, we tend to get stuck in build mode. Our cells keep trying to grow when they should be repairing. This is one reason chronic overeating—even healthy foods—may accelerate aging at the cellular level.
The research is striking: animals with reduced "build mode" signaling live significantly longer.
The Practical Takeaway¶
You don't need to understand the biochemistry to coach effectively. Here's what matters:
- Eat adequate protein at meals to maintain muscle
- Don't eat constantly—allow time between meals for repair mode
- Chronic overeating accelerates aging, regardless of food quality
That's why what you eat and how much both matter for longevity.
For the full biochemistry (mTOR, AMPK, sirtuins), see the Deep Dive: How Food Affects Aging Biology.
[CHONK: The Mediterranean and MIND Approach]
The Mediterranean and MIND Approach¶
If you read longevity research, one dietary pattern appears again and again: the Mediterranean diet. It's not the only healthy way to eat, but it has the strongest evidence base for longevity outcomes.
Why a Dietary Pattern, Not a "Diet"¶
First, let's be clear: we're talking about a pattern of eating, not a restrictive diet with forbidden foods. The Mediterranean approach describes what people in Mediterranean regions traditionally ate, not a commercial program with rules and phases.
Why this matters:
- No single diet works for everyone. Cultural background, food access, preferences, and health conditions all affect what's realistic.
- Patterns are sustainable; restrictions aren't. Clients can adopt Mediterranean principles while still eating foods they love.
- The whole pattern matters more than individual foods. No single "superfood" drives the benefits. It's the combination.
What Is the Mediterranean Diet?¶
The Mediterranean dietary pattern emphasizes:
- Vegetables in abundance: 6-10 servings daily, with variety and color
- Fruits: Especially berries and other whole fruits
- Whole grains: Bread, pasta, rice, minimally processed
- Legumes: Beans, lentils, chickpeas, protein and fiber sources
- Nuts and seeds: Especially almonds, walnuts, and seeds
- Olive oil: As the primary fat source, especially extra-virgin
- Fish and seafood: 2-3 times weekly, especially fatty fish
- Moderate dairy: Cheese and yogurt in moderation
- Limited red meat: A few times monthly rather than daily
- Moderate wine: Traditionally included, though we'll discuss alcohol separately
The Evidence for Longevity¶
The evidence is substantial:
The Women's Health Study followed over 25,000 U.S. women for approximately 25 years. Those with the highest Mediterranean diet adherence had 23 percent lower all-cause mortality compared to those with lowest adherence (JAMA Network Open, 2024).
PREDIMED, a landmark randomized trial of nearly 7,500 high-risk adults, found that those assigned to a Mediterranean diet supplemented with extra-virgin olive oil or nuts had about 30 percent fewer major cardiovascular events (heart attacks, strokes, cardiovascular deaths) compared to a low-fat control group over roughly five years (NEJM, 2013; Advances in Nutrition, 2014).
Meta-analyses across 29 cohorts showed a linear, dose-response relationship: the more closely people followed Mediterranean principles, the lower their mortality risk. Even modest increases in adherence conferred benefits (Advances in Nutrition, 2019).
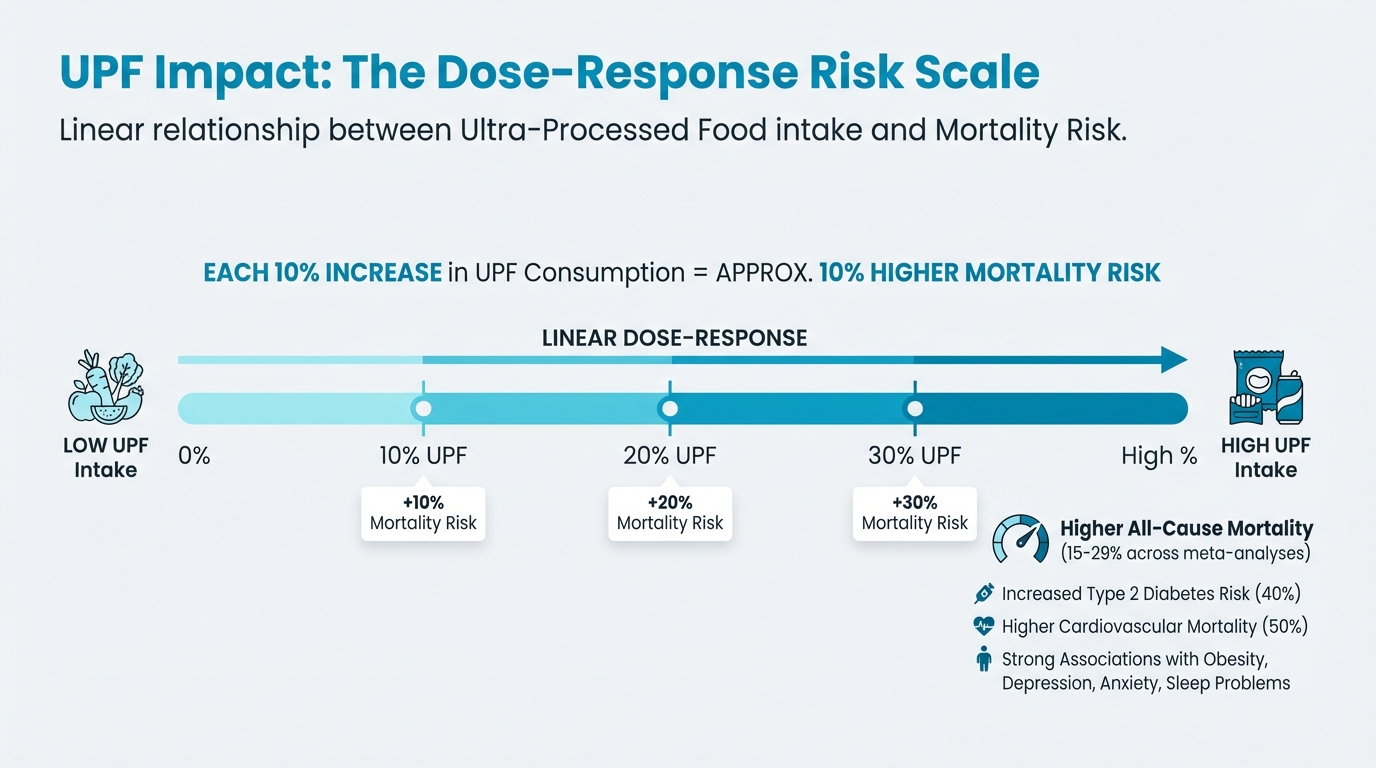
Figure: Dose-response relationship (10% increase = 10% mortality)
Mechanisms: The benefits appear to work through reduced inflammation, improved lipid profiles (cholesterol), lower insulin resistance, better body composition, and even slower epigenetic aging. One trial found that higher Mediterranean adherence reduced "epigenetic age acceleration" by approximately 1.4 years (Nutrients, 2024).
The MIND Diet: Mediterranean Meets Brain Health¶
The MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) was specifically designed to support cognitive health. It combines elements of the Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets, with emphasis on foods linked to brain health:
Brain-healthy foods emphasized:
- Leafy green vegetables (at least 6 servings weekly)
- Other vegetables (at least 1 daily)
- Berries (at least 2 servings weekly)
- Nuts (5+ servings weekly)
- Olive oil (as primary cooking fat)
- Whole grains (3+ servings daily)
- Fish (at least 1 weekly)
- Beans (4+ meals weekly)
- Poultry (2+ meals weekly)
Foods to limit:
- Red meat (fewer than 4 servings weekly)
- Butter/margarine (less than 1 tablespoon daily)
- Cheese (less than 1 serving weekly)
- Pastries and sweets (fewer than 5 weekly)
- Fried/fast food (fewer than 1 weekly)
The evidence for cognition: In a 2025 systematic review of 18 studies, 16 reported cognitive benefits with higher MIND adherence, particularly for global cognition, memory, and executive function (Journal of Nutrition, Health & Aging, 2025). The Rotterdam Study found 15-24 percent lower dementia risk with higher MIND scores over 5-7 years (Alzheimer's Research & Therapy, 2022).
Neuropathology studies add biological plausibility: higher MIND adherence is associated with lower odds of hippocampal sclerosis and neuronal loss at autopsy (JAMA Network Open, 2025).
Practical Implementation¶
How do you help clients actually eat this way?
Start with addition, not restriction:
- "What vegetables could you add to dinner this week?"
- "Could you try fish once or twice instead of your usual protein?"
- "What if you switched to olive oil for cooking?"
Cultural adaptation matters:
- Mediterranean principles work across cuisines. Asian, Latin American, and African food traditions can all align with these principles.
- The goal is the pattern—vegetables, legumes, fish, olive oil, whole grains—not specific Greek or Italian dishes.
Make it practical:
- Canned beans count, and so do frozen vegetables and jarred olive oil.
- Perfect isn't the goal; consistent is.
| Coaching in Practice | |
|---|---|
| Conversation starter for Mediterranean principles: "Looking at your typical week, what would happen if we just focused on adding more vegetables and switching your cooking oil to olive oil? We're not taking anything away. Just adding some things that research shows matter for long-term health." |
| Coaching in Practice | |
|---|---|
| Common client objection: "I don't like Mediterranean food" Your response: "Good news, Mediterranean eating isn't about specific dishes like falafel or Greek salads. It's about principles: more vegetables, olive oil instead of butter, fish a couple times a week, beans and legumes, nuts for snacks. You can apply those principles to any cuisine. What foods do you already enjoy that fit these patterns? Let's start there." |
| Coaching in Practice | |
|---|---|
| Practical grocery list for Mediterranean principles: Help clients start with these staples: Extra-virgin olive oil (primary cooking fat), canned chickpeas and beans, frozen vegetables, nuts (walnuts, almonds), canned or frozen fish (salmon, sardines), whole grains (quinoa, brown rice, whole wheat pasta), fresh or frozen berries. These items are affordable, have long shelf life, and form the backbone of Mediterranean eating. |
What This Means for Your Client¶
When you recommend Mediterranean principles, you're not just giving diet advice, you're helping clients adopt an eating pattern with decades of research behind it showing reduced mortality, cardiovascular protection, and cognitive benefits. The evidence is strong enough that you can say confidently: "This is what the research consistently shows works for long-term health."
[CHONK: Protein for Longevity: Preventing Sarcopenia]
Protein for Longevity: Keeping Muscle as You Age¶
Here's a number that gets people's attention: by age 80, many people have lost 30-40 percent of their muscle mass. This condition—called sarcopenia—is a major driver of frailty, falls, and loss of independence.
The good news? It's largely preventable with adequate protein and resistance training.
Why Muscle Matters¶
Muscle isn't just for athletes:
- It regulates blood sugar (muscle is where glucose goes after meals)
- It provides reserves during illness (your body draws on muscle for recovery)
- It predicts independence (grip strength predicts fall risk and mortality)
The Practical Targets¶
Forget the numbers for a moment. Here's what matters:
A palm-sized portion of protein at each meal. That's roughly 25-35 grams—enough to tell your muscles to maintain themselves.
Breakfast is the biggest opportunity. Most people eat almost no protein at breakfast (coffee and toast, maybe 10 grams). That's the longest gap since eating, and exactly when muscles could benefit. Adding eggs, Greek yogurt, or cottage cheese to breakfast is one of the highest-impact changes you can recommend.
Spread it across the day. Eating 80 grams at dinner isn't as effective as eating 30 grams at three meals. Your muscles can only use so much at once.
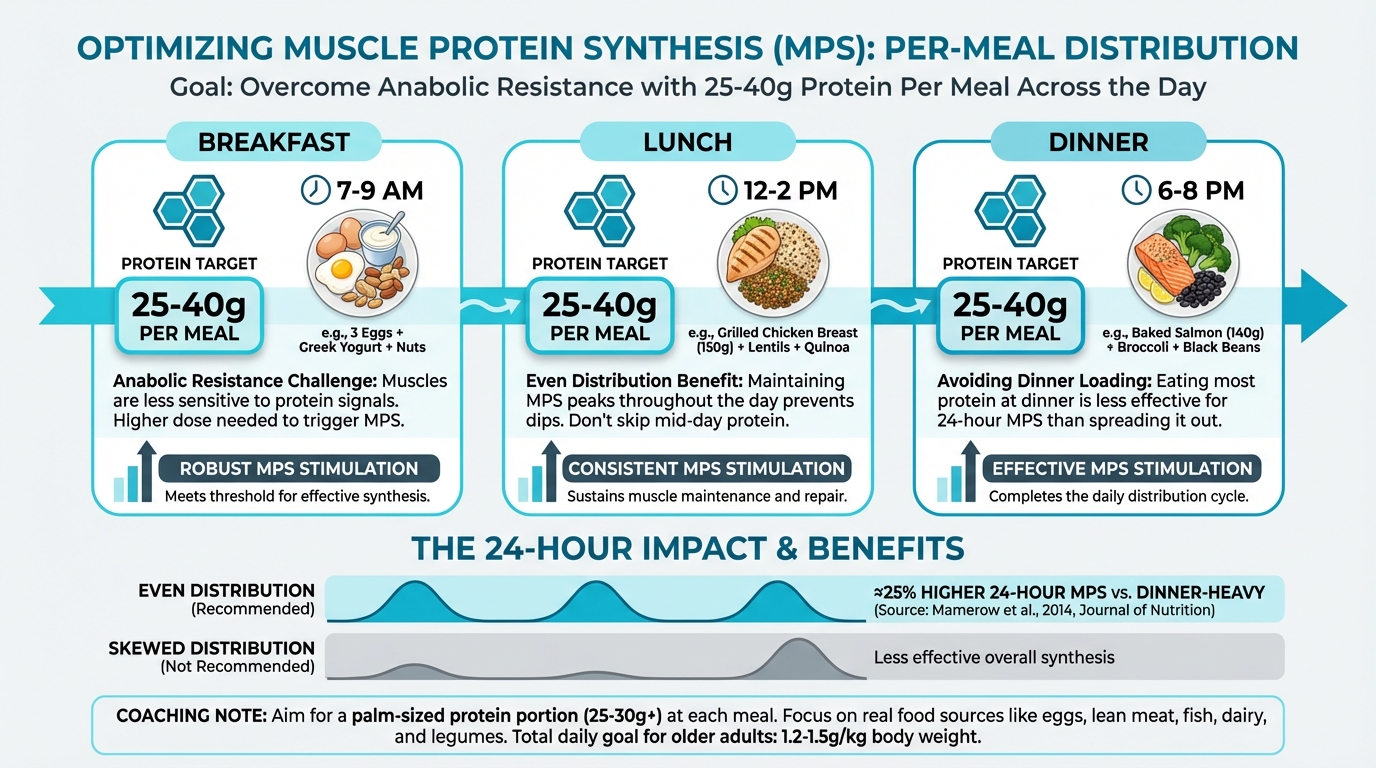
Figure: Protein distributed across meals works better than loading it all at dinner
Plant-Based? You'll Need a Bit More¶
Plant proteins work fine, but you need larger portions to get the same muscle-building signal. Prioritize soy (tofu, tempeh, edamame) and combine proteins (beans + grains). A plant-based client might need a slightly larger palm-sized portion at each meal.
For the detailed research (g/kg requirements, leucine thresholds, anabolic resistance), see the Deep Dive: Protein Requirements Research.
What This Means for Coaching¶
| Coaching in Practice | |
|---|---|
| Protein tracking without obsession: Help clients estimate protein without becoming compulsive. A simple approach: "Aim for a palm-sized portion of protein at each meal (about 25-30g), and make sure breakfast includes real protein, not just carbs." For those who want precision, tracking for 3-5 days can reveal patterns without becoming a permanent requirement. |
| Coaching in Practice | |
|---|---|
| The "protein audit" conversation: "Let's do a quick protein audit. Walk me through yesterday, what did you eat for breakfast? Lunch? Dinner? Any snacks?" As they share, mentally estimate protein at each meal. Most clients will reveal a pattern: little protein at breakfast (5-15g), moderate at lunch (15-25g), and most at dinner (40-50g). This skewed pattern is incredibly common and represents a big opportunity. |
| Coaching in Practice | |
|---|---|
| Addressing the "I'm not hungry for breakfast" client: Many clients skip breakfast or eat lightly. Explore the root cause: Is it habit? Time pressure? Genuine lack of appetite? For those genuinely not hungry, suggest: "Start small. Even 15-20 grams is better than zero. Try Greek yogurt or a couple of eggs. Your appetite in the morning often increases once you establish the habit. We can build up to 30+ grams over a few weeks." |
What About Plant-Based Clients?¶
Plant-based eating is entirely compatible with adequate protein for longevity, but it requires more intentionality:
Leucine content matters: Plant proteins generally contain less leucine per gram of protein. To hit the leucine threshold, plant-based clients need larger protein portions or strategic combinations.
Best plant protein sources for leucine:
- Soy products (tofu, tempeh, edamame): highest plant leucine content
- Legumes combined with grains
- Seitan (wheat gluten)
- Quinoa (complete protein)
Practical approach: A plant-based client might need 40-50g of plant protein per meal to achieve the same muscle protein synthesis stimulus as 30g of animal protein. This is achievable but requires planning.
| For DIY Learners |
|---|
| Applying this to yourself: Do a quick protein audit of your own typical day. Walk through yesterday: What did you eat for breakfast? How much protein was in it? What about lunch and dinner? Most people discover the same pattern: almost nothing at breakfast, light at lunch, heavy at dinner. If that's you, try adding just 20 grams to breakfast this week—Greek yogurt, eggs, or a protein shake. It's one of the highest-impact nutrition changes for longevity. |
[CHONK: Fiber, Plants, and the Microbiome]
Fiber, Plants, and the Microbiome¶
If protein is about maintaining structure, fiber and plant diversity are about maintaining systems, particularly your gut microbiome and the inflammatory environment throughout your body.
Fiber Targets: 30-50 Grams Daily¶
Most people don't come close. The average American consumes about 15 grams of fiber daily, half the minimum recommendation and far below the 30-50 grams associated with optimal health outcomes.
Why fiber matters for longevity:
- Feeds beneficial gut bacteria that produce short-chain fatty acids (SCFAs), which reduce inflammation and support gut barrier function
- Lowers cholesterol by binding bile acids
- Improves blood sugar control by slowing digestion
- Promotes regular elimination and reduces colon cancer risk
The 6-10 Servings Guideline¶
The protocol recommends 6-10 servings of colorful vegetables daily. That sounds like a lot, but a "serving" is about half a cup cooked or one cup raw.
Why color diversity matters:
Different colors indicate different phytonutrients: plant compounds with antioxidant and anti-inflammatory effects:
- Reds (tomatoes, red peppers): lycopene
- Oranges (carrots, sweet potatoes): beta-carotene
- Greens (leafy vegetables, broccoli): folate, vitamin K
- Purples/blues (berries, eggplant): anthocyanins
- Whites (garlic, onions): allicin
The goal isn't perfection, it's diversity. Different plant compounds feed different microbial populations, and microbiome diversity is associated with better health outcomes.
The Microbiome Connection¶
Your gut houses trillions of bacteria that influence:
- Inflammation throughout your body
- Immune function
- Neurotransmitter production (gut-brain axis)
- Nutrient absorption
- Even your weight regulation
A fiber-rich, plant-diverse diet promotes a healthy microbiome. Ultra-processed foods, antibiotics, and low-fiber diets do the opposite.
Practical Strategies¶
Add, don't restrict:
- Add a side salad to lunch
- Include vegetables with breakfast (spinach in eggs, tomatoes alongside)
- Keep frozen vegetables for easy additions
- Add beans to soups, salads, and grain dishes
Increase gradually:
- Rapid fiber increases cause bloating and gas
- Add 5 grams per week until reaching target
- Drink adequate water as fiber increases
Prioritize diversity over perfection:
- Aim for 30 different plant foods weekly (this sounds like a lot, but includes vegetables, fruits, whole grains, legumes, nuts, seeds, herbs, and spices)
- Variety matters more than hitting exact targets
| Coaching in Practice | |
|---|---|
| Fiber gradual increase protocol: "Rather than overhauling your diet overnight, let's add fiber gradually. This week, could you add one extra serving of vegetables to your day, maybe a side salad at lunch or an extra handful of vegetables at dinner? Next week, we'll add another. Your gut bacteria need time to adjust, and going slow prevents the bloating that makes people quit." |
The "30 Different Plants" Challenge¶
Research on the microbiome suggests that diversity matters as much as quantity. A landmark study from the American Gut Project found that people who ate 30 or more different plant foods per week had more diverse gut microbiomes than those who ate fewer than 10.
What counts as a "plant food":
- Vegetables (each type counts separately, spinach and kale are two plants)
- Fruits
- Whole grains (oats, rice, quinoa each count)
- Legumes (chickpeas, black beans, lentils each count)
- Nuts and seeds (almonds, walnuts, chia seeds each count)
- Herbs and spices (yes, basil, oregano, and turmeric count!)
When you include herbs and spices, hitting 30 plants weekly becomes much more achievable. This is a great reframe for clients who feel overwhelmed: "You're probably already eating more plant diversity than you realize. Let's count it up."
| Coaching in Practice | |
|---|---|
| The diversity conversation: "Here's something interesting from the research: eating a variety of plants matters as much as the total amount. Different plants feed different gut bacteria, and diversity in your microbiome is linked to better health. The target is about 30 different plant foods per week. That sounds like a lot, but when you count herbs and spices—basil counts, turmeric counts—you're probably closer than you think. Want to try tracking it for a week just to see where you are?" |
Why Clients Struggle With Vegetables¶
Understanding barriers helps you coach more effectively:
Taste preferences: Many adults grew up with overcooked, unseasoned vegetables. Help them discover that roasted vegetables with olive oil and salt taste dramatically different from boiled broccoli.
Convenience: Vegetables require washing, chopping, and cooking. Frozen vegetables, pre-cut options, and roasting large batches help.
Habit: If someone has eaten the same meals for years, vegetables feel like an addition rather than a default. Building new routines takes time.
Cost perception: Fresh vegetables can seem expensive. Frozen vegetables, canned beans, and seasonal produce are affordable alternatives with equivalent nutrition.
[CHONK: What to Limit: Evidence-Based Guidance]
What to Limit: Evidence-Based Guidance¶
Longevity nutrition isn't just about what to add. There are also foods and substances worth reducing. The key is presenting this honestly without creating food fear or orthorexic anxiety.
Ultra-Processed Foods (UPFs)¶
What they are: The NOVA classification defines ultra-processed foods as industrial formulations made mostly from substances derived from foods plus additives. Think: packaged snacks, sweetened beverages, instant noodles, many breakfast cereals, reconstituted meat products.
The evidence is substantial:
- Highest vs. lowest UPF intake is associated with 15-29 percent higher all-cause mortality across multiple meta-analyses (Liang et al., 2025; American Journal of Epidemiology, 2022)
- 40 percent higher type 2 diabetes risk (Frontiers in Nutrition, 2024)
- 50 percent higher cardiovascular mortality with convincing evidence (BMJ umbrella review, 2024)
- Strong associations with obesity, depression, anxiety, and sleep problems
Not all UPFs are equal:
- Processed meats and sugar-sweetened beverages show the strongest harmful associations
- Some UPF categories (like certain fortified breakfast cereals) show neutral or even inverse associations
- The dose-response is linear: each 10 percent increase in UPF consumption is linked to approximately 10 percent higher mortality risk
The coaching approach:
- Focus on reduction, not elimination. Perfection isn't the goal
- Help clients identify their highest-impact swaps (replacing daily soda has more impact than worrying about occasional packaged crackers)
- Emphasize adding whole foods, which naturally displaces UPFs
Added Sugars and Sugar-Sweetened Beverages¶
Sugar-sweetened beverages are the single most consistently harmful category in nutrition research. They provide calories without satiation, spike blood sugar, and are associated with metabolic disease risk.
Practical targets:
- Limit added sugars to less than 10 percent of calories (about 50 grams for a 2,000-calorie diet)
- Replace sweetened beverages with water, unsweetened tea/coffee, or sparkling water
- Read labels. Sugar hides in sauces, dressings, and "healthy" packaged foods
Saturated Fat: Context Matters¶
The recommendation to keep saturated fat below 10 percent of calories is based on its effects on LDL cholesterol and cardiovascular risk. But context matters:
- Quality matters: Saturated fat from whole foods (eggs, full-fat dairy) appears less harmful than from processed foods
- Replacement matters: Replacing saturated fat with refined carbohydrates doesn't improve outcomes; replacing with unsaturated fats (olive oil, nuts, fish) does
- Individual variation exists: Some people's cholesterol responds more to dietary saturated fat than others
The practical approach:
- Use olive oil as primary cooking fat
- Don't obsess over every gram of saturated fat
- If cardiovascular risk is elevated (high ApoB), saturated fat reduction becomes more important
Avoiding Food Fear¶
Here's the challenge: too much focus on "bad" foods creates anxiety that may be worse than the foods themselves.
The 80/20 principle:
- If 80 percent of someone's diet consists of whole, minimally processed foods, the other 20 percent matters much less
- Occasional pizza, birthday cake, or restaurant meals don't derail longevity
- Social eating and food enjoyment are part of Deep Health
Language matters:
- "Foods to eat less often" rather than "bad foods"
- "Let's focus on adding these foods" rather than "you need to eliminate these"
- "How does eating this way make you feel?" rather than "this food is toxic"
| Coaching in Practice | |
|---|---|
| The "swap" conversation instead of "eliminate": "I notice you're eating packaged granola bars as snacks most days. Those are pretty processed: lots of added sugar and not much protein. What if we experimented with some alternatives? A handful of nuts and an apple? Greek yogurt? You don't have to give up the granola bars entirely, but what if they became the backup option instead of the default?" |
Identifying High-Impact Swaps¶
Not all UPF reduction is equal. Focus coaching on the highest-impact changes:
High impact (worth prioritizing):
- Sugar-sweetened beverages → water, unsweetened tea, sparkling water
- Processed meats (daily) → fish, poultry, legumes
- Packaged snacks → nuts, vegetables, whole fruit
- Sweetened breakfast cereals → oatmeal, eggs, Greek yogurt
Lower impact (don't obsess):
- Occasional condiments with added sugar
- Whole grain bread (technically processed, but beneficial)
- Plain crackers with whole food toppings
Help clients distinguish between "ultra-processed" and "any processing." All cooking is processing. The concern is industrial formulations designed for hyper-palatability, not foods that simply come in packages.
[CHONK: Alcohol: The Honest Conversation]
Alcohol: The Evidence Coaches Need to Know¶
Alcohol deserves its own section because the evidence has shifted significantly in recent years, and coaches need accurate information to have honest conversations with clients.
The Old Story vs. The New Evidence¶
The old story (what many clients believe): Moderate drinking, especially red wine, is good for your heart. The "J-curve" showed that moderate drinkers lived longer than abstainers.
The new evidence (what research now shows): When researchers controlled for biases in those earlier studies, the apparent protective effect largely disappeared.
A 2023 meta-analysis in JAMA Network Open pooled 107 cohort studies (4.84 million participants) and found:
- No statistically significant mortality benefit for low-to-moderate drinking compared to lifetime abstainers
- Occasional drinkers (<1.3 g/day): RR 0.96 (95% CI 0.86–1.06). Not significant
- Low-volume drinkers (1.3–24 g/day): RR 0.93 (P=0.07). Not significant
- Higher consumption increased mortality (45–64 g/day: RR 1.19; ≥65 g/day: RR 1.35)
(Zhao et al., 2023, JAMA Network Open)
Why the J-Curve Was Wrong¶
The apparent "protection" from moderate drinking was largely driven by methodological problems:
Sick quitter bias: Many "abstainers" in studies were former drinkers who quit due to health problems. Comparing current moderate drinkers to this unhealthy group made drinkers look healthier.
Healthy user bias: Moderate drinkers tend to be wealthier, more educated, and have healthier lifestyles overall. The "benefit" may have been confounded by these factors.
Mendelian randomization (using genetic variants as natural experiments) does not confirm cardiovascular benefits from moderate drinking (Tsai & Gao, 2023, BMC Medicine).
The Cancer Issue¶
Even if cardiovascular effects are debated, cancer risk is clear:
There is no safe level of alcohol for cancer risk. Even very moderate intake increases risk for:
- Breast cancer
- Oral and throat cancers
- Esophageal cancer
- Colorectal cancer
The WHO Regional Office for Europe states explicitly: "There is no safe amount of alcohol that does not affect health" (WHO, 2023).
The National Academies of Sciences, Engineering, and Medicine (NASEM) 2025 report concludes: "Drinking less is better than drinking more" and advises not to start drinking for health benefits.
How to Talk About This With Clients¶
This is where coaching skill matters. You're not the alcohol police, and prohibition messaging often backfires. Here's a framework:
For coaches (what you need to understand):
- The evidence no longer supports "moderate drinking is healthy"
- Any amount increases cancer risk
- The "tolerable risk" is low. The protocol suggests 0-4 drinks/week maximum, with less being better
- Some people will choose to drink despite the risks, and that's their choice to make
For client conversations:
| Coaching in Practice | |
|---|---|
| When a client asks: "Is it okay to have a glass of wine with dinner?" A balanced response: "The honest answer from recent research is that there's no health benefit from alcohol, and any amount slightly increases some cancer risks. If you enjoy wine with dinner occasionally and it's part of social connection for you, a glass a few times a week represents a fairly small risk. The research suggests keeping it under 4 drinks per week, and honestly, less is better. But you're an adult making informed choices. I just want you to have the accurate information." |
For clients who drink more heavily:
- This is a medical and sometimes psychological issue beyond coaching scope
- If someone reports drinking daily or in larger quantities, this warrants referral
- Focus on harm reduction rather than judgment
Practical guidance for those who choose to drink:
- 0-2 drinks/week: Minimal risk
- 3-4 drinks/week: Small but real increase in risk. The upper limit for "tolerable"
- 7+ drinks/week: Clearly elevated risk; recommend reduction
- Daily drinking or binge patterns: Referral territory
Sex Differences and Context¶
The evidence shows some important variations:
Women face higher cancer risk from alcohol: Breast cancer risk increases even at low intake levels. One drink daily may increase breast cancer risk by 5-10 percent.
Binge drinking is worse than spread consumption: Four drinks on Saturday is worse than one drink on four separate days, even though the total is the same.
Age matters: The relative risks of alcohol may shift with age. In younger people, alcohol contributes to accidents and risky behavior. In older adults, fall risk and medication interactions become concerns.
What Not to Say¶
Avoid these coaching mistakes:
- Don't moralize: "You really shouldn't drink at all" rarely helps and can damage the coaching relationship.
- Don't dismiss concerns: If a client asks about alcohol, they're probably already thinking about it. Take the question seriously.
- Don't oversimplify: "A little is fine" or "any amount is poison" are both inaccurate. Present the nuance.
- Don't push beyond scope: If someone has alcohol dependence or is using alcohol to cope with emotional issues, this needs medical/psychological support, not coaching.
| Coaching in Practice | |
|---|---|
| When a client reports drinking more than the tolerable threshold: "I appreciate you being honest with me about that. The research is pretty clear that at 10-15 drinks per week, the health risks start adding up significantly. I'm not here to judge. I am here to give you accurate information. Would it be helpful to talk about what role alcohol plays in your life and whether there are changes you'd want to make? If this feels bigger than just a nutrition habit, I can also help connect you with someone who specializes in this area." |
[CHONK: Supplements: Scope-Appropriate Guidance]
Supplements: Staying Within Scope¶
Supplements are where coaches most often overstep their scope. Let's be crystal clear on boundaries (review Chapter 1.5 if needed):
Coaches CAN:
- Educate about what supplements are and how they're regulated
- Share general evidence about supplement categories
- Help clients implement recommendations from their healthcare provider
- Suggest clients discuss specific supplements with their doctor or dietitian
Coaches CANNOT:
- Recommend specific supplements, brands, or dosages
- Diagnose nutrient deficiencies
- Suggest supplements to treat health conditions
- Sell supplements to clients (major conflict of interest and scope violation)
The "From Diet First" Principle¶
The protocol emphasizes that supplements supplement. They don't replace a good diet. For most people, a Mediterranean-style eating pattern provides adequate nutrients without supplementation.
Nutrition-Related Supplements Worth Knowing About¶
Omega-3s (EPA/DHA): If clients don't eat fatty fish 2-3 times weekly, omega-3 supplementation (2-3g combined EPA/DHA daily) may fill the gap. Evidence supports cardiovascular and anti-inflammatory benefits.
Vitamin D: Many people are deficient, especially those living at northern latitudes, with dark skin, or who spend little time outdoors. The protocol targets 40-60 ng/mL blood levels. Common supplementation: 2,000-5,000 IU daily depending on starting levels. Testing is recommended.
Fiber supplements (psyllium): If dietary fiber intake is insufficient despite efforts, psyllium can help reach targets. It's food-derived and low-risk.
Teaching Clients About Supplement Quality¶
Since you can't recommend specific brands, teach clients what to look for:
Third-party testing certifications:
- USP (United States Pharmacopeia): Tests for identity, strength, purity, and dissolution
- NSF International: Certifies products meet label claims and are free from contaminants
- ConsumerLab: Independent testing with published results
- Informed Sport/Informed Choice: Tests for banned substances (relevant for athletes)
Red flags:
- Products making dramatic health claims ("cures," "reverses aging")
- Products that are dramatically cheaper than competitors
- Products without any third-party verification
- Products sold through multi-level marketing
The conversation:
"I can't recommend specific brands, but I can tell you what to look for. Check the label for third-party testing seals like USP or NSF. These organizations verify that what's on the label is actually in the bottle and that it's free from contaminants."
[CHONK: Deep Health Integration]
Deep Health Integration¶
Nutrition affects every dimension of Deep Health, not just the physical. Here's how:
Physical: This is obvious. Nutrition directly affects metabolic health, body composition, energy levels, and disease risk. It's the primary focus of this chapter.
Emotional: How someone eats affects how they feel about eating. Restrictive diets, food guilt, and constant monitoring can damage emotional health even while "improving" nutrition. Your job is to help clients develop a healthy, enjoyable relationship with food, not anxiety.
Social: Food is fundamentally social. Shared meals connect us to family, friends, and culture. Overly rigid nutrition rules can isolate people from social eating. Help clients find approaches that support health while preserving connection.
Environmental: Where food comes from matters to some clients. Sustainable sourcing, reducing food waste, and supporting local food systems are valid concerns. Meet clients where they are on these issues.
Mental: The MIND diet evidence reminds us that nutrition directly affects brain function. Blood sugar stability affects focus and mood. Omega-3s support neurological health.
Existential: How does someone want to eat for the rest of their life? Nutrition for longevity should align with their values and vision, not just hit macronutrient targets.
[CHONK: Coaching in Practice: A Sample Day]
Coaching in Practice: Putting It Together¶
Case Study: Marcus, 47¶
Background: Marcus is a busy marketing executive who wants to "eat for longevity" after his father's recent heart attack. He currently skips breakfast, grabs lunch from nearby restaurants, and eats a large dinner with 2-3 glasses of wine most nights. He's interested but overwhelmed by all the information.
Assessment findings:
- Protein intake: ~70g daily (mostly at dinner)
- Fiber intake: ~12g daily
- Vegetable servings: 1-2 daily
- Alcohol: 15-20 drinks/week
- UPF consumption: Moderate (packaged snacks, some processed meats)
Priority setting: Where do we start?
- Alcohol (highest immediate risk, client receptive to discussion given father's heart attack)
- Protein distribution (adding breakfast protein)
- Vegetable addition (increase without major lifestyle changes)
- UPF reduction (gradual, focused on highest-impact swaps)
A Sample Day (Illustrative, Not Prescriptive)¶
This example shows Mediterranean/MIND principles, adequate protein distribution, and fiber targets. Adapt to your clients' preferences, cultural background, and food access.
Breakfast (~500 calories, ~35g protein, ~8g fiber)
- Greek yogurt (1.5 cups) with walnuts, blueberries, and ground flaxseed
- Coffee with splash of milk
Lunch (~600 calories, ~35g protein, ~12g fiber)
- Large mixed salad with chickpeas, grilled chicken, olive oil/lemon dressing
- Whole grain bread
- Apple
Afternoon snack (~200 calories, ~10g protein, ~5g fiber)
- Hummus with raw vegetables (carrots, cucumbers, bell peppers)
Dinner (~700 calories, ~40g protein, ~15g fiber)
- Grilled salmon with olive oil and herbs
- Roasted vegetables (broccoli, sweet potato, onions)
- Side salad with mixed greens
- Quinoa or whole grain
- Glass of wine (optional, 1 night per week instead of nightly)
Daily totals (approximate):
- Protein: ~120g (distributed ~35/35/10/40)
- Fiber: ~40g
- Vegetables: 8+ servings
- Omega-3s: High (salmon, walnuts, flaxseed)
- Olive oil: Primary fat
- Alcohol: Reduced from 3/night to occasional
Disclaimer: This is an illustrative example showing how the principles come together, not a prescription. Individual needs vary based on body size, activity level, health conditions, and preferences. Clients with specific medical conditions should work with a registered dietitian.
Phased Implementation¶
Month 1: Foundation
- Add protein to breakfast (primary focus)
- Reduce alcohol to 4 drinks/week maximum
- One coaching conversation about why these matter
Month 2: Building
- Add vegetables to two meals daily
- Introduce meal prep strategies
- Continue alcohol reduction if needed
Month 3: Refining
- Work on fiber diversity
- Address UPF swaps
- Fine-tune based on what's working
Sample Coaching Conversation¶
Here's how a conversation about nutrition for longevity might flow:
Coach: "Marcus, you mentioned wanting to eat for longevity after your dad's heart attack. Before we dive into specifics, what does eating well look like to you? What's already working?"
Marcus: "I don't know, honestly. I feel like I should be doing more. I've read about all these diets—keto, Mediterranean, intermittent fasting—and I don't know where to start."
Coach: "That overwhelm is totally normal, there's so much information out there. Here's what I can tell you: the research consistently points to a few things that matter most. Adequate protein to maintain muscle as you age, lots of vegetables and fiber, mostly whole foods rather than packaged stuff, and being honest about alcohol. Does that feel more manageable than picking a specific diet?"
Marcus: "Yeah, that's more doable. But where do I start?"
Coach: "Let's pick one thing. Looking at your typical day, I notice you skip breakfast and then load up at dinner. One high-impact change would be adding protein to your morning. What feels realistic? Could you do eggs a few days a week? Or grab some Greek yogurt?"
Marcus: "I could probably do eggs. I'm just not hungry in the morning."
Coach: "That's common when you've trained your body to skip breakfast. Start small. Even two eggs is a good start, about 12-14 grams of protein. Once that becomes routine, we can build up. Does that work as our focus for the next two weeks?"
Common Pitfalls to Avoid¶
As you coach nutrition for longevity, watch for these traps:
The perfectionism trap: Clients who try to change everything at once typically burn out. Start with one or two changes and build.
The optimization obsession: Some clients get so focused on optimizing that they miss the basics. If someone's asking about meal timing while eating fast food daily, redirect to fundamentals.
The fear-based approach: Presenting nutrition as avoiding "bad" foods creates anxiety. Lead with addition—what to include—not just what to avoid.
The scope creep: It's tempting to give specific supplement recommendations or interpret lab results when clients ask. Stay within scope and refer appropriately.
[CHONK: Study Guide Questions]
Study Guide Questions¶
These questions help you review the chapter and prepare for the exam. They're optional but recommended.
-
How do nutrient-sensing pathways (mTOR, AMPK) connect nutrition to aging biology? How does this inform the recommendation to avoid chronic caloric excess?
-
What are the key components of the Mediterranean dietary pattern, and what does the evidence show about its effects on mortality and cardiovascular outcomes?
-
Why do older adults need more protein than the standard RDA? What are the per-meal targets, and why does distribution matter?
-
What is the current evidence regarding alcohol and health? How would you explain this to a client who believes moderate drinking is protective?
-
How would you help a client reduce ultra-processed foods without creating food fear or an all-or-nothing approach?
-
What CAN and CANNOT coaches do regarding supplement recommendations? How would you handle a client asking you what supplements to take?
Self-reflection questions:
-
Do a quick protein audit of your own typical day. How much protein do you get at breakfast? Lunch? Dinner? Where could you improve protein distribution?
-
How much of your diet comes from ultra-processed foods? What's one swap you could make this week to shift toward more whole foods?
Deep Dives¶
Want to go deeper? These supplemental articles explore key topics from this chapter in more detail.
- How Food Affects Aging Biology: The mTOR, AMPK, and sirtuin pathways explained
- Protein Requirements Research: The detailed science behind protein targets
- Microbiome Science: The gut-longevity connection in depth
- Supplement Evidence Review: Omega-3, Vitamin D research
References¶
-
Ahmad S, Moorthy MV, Lee I, Ridker PM, Manson JE, Buring JE, et al. Mediterranean Diet Adherence and Risk of All-Cause Mortality in Women. JAMA Network Open. 2024;7(5):e2414322. doi:10.1001/jamanetworkopen.2024.14322
-
Unknown. Mediterranean diet lowers all-cause and cardiovascular mortality for patients with metabolic syndrome. Diabetology & Metabolic Syndrome; 2023. https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-023-01052-7
-
Adherence to the Mediterranean Diet in Relation to All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis. Adherence to the Mediterranean Diet in Relation to All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis. Advances in Nutrition; 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6855973/
-
Ros E, Martínez-González MA, Estruch R, Salas-Salvadó J, Fitó M, Martínez JA, et al. Mediterranean Diet and Cardiovascular Health: Teachings of the PREDIMED Study. Advances in Nutrition. 2014;5(3):330S-336S. doi:10.3945/an.113.005389
-
Mediterranean Diet for Primary Prevention of Cardiovascular Disease. New England Journal of Medicine. 2014;370(14):1368-1368. doi:10.1056/nejmx140016
-
Unknown. Molecular Mechanisms of Healthy Aging: CR, Fasting, Mediterranean and Ketogenic Diets.. Nutrients; 2024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11397047/
-
Wang VH, GU Y, Gelman A, Divers J, Zhang D. Abstract P2100: Longitudinal association between MIND diet adherence, inflammatory mechanism, and cognitive health. Circulation. 2025;151(Suppl_1). doi:10.1161/cir.151.suppl_1.p2100
-
MIND diet and the risk of dementia: a population-based study. MIND diet and the risk of dementia: a population-based study. Alzheimer's Research & Therapy; 2022. https://pmc.ncbi.nlm.nih.gov/articles/PMC8756695/
-
Agarwal P, Agrawal S, Wagner M, Cherian LJ, Aggarwal NT, James BD, et al. MIND Diet and Hippocampal Sclerosis Among Community-Based Older Adults. JAMA Network Open. 2025;8(8):e2526089. doi:10.1001/jamanetworkopen.2025.26089
-
Lee E, Kim I, Lim S. Physical activity and protein-intake strategies to prevent sarcopenia in older people. International Health. 2025;17(4):423-430. doi:10.1093/inthealth/ihae064
-
N/A. Dietary protein requirements of older adults with sarcopenia. Frontiers in Nutrition; 2025. https://pmc.ncbi.nlm.nih.gov/articles/PMC11906324
-
Coelho-Júnior HJ, Calvani R, Tosato M, Landi F, Picca A, Marzetti E. Protein intake and physical function in older adults: A systematic review and meta-analysis. Ageing Research Reviews. 2022;81:101731. doi:10.1016/j.arr.2022.101731
-
Mamerow MM, Mettler JA, English KL, Casperson SL, Arentson-Lantz E, Sheffield-Moore M, et al. Dietary Protein Distribution Positively Influences 24-h Muscle Protein Synthesis in Healthy Adults. The Journal of Nutrition. 2014;144(6):876-880. doi:10.3945/jn.113.185280
-
Taneri PE, Wehrli F, Roa-Díaz ZM, Itodo OA, Salvador D, Raeisi-Dehkordi H, et al. Association Between Ultra-Processed Food Intake and All-Cause Mortality: A Systematic Review and Meta-Analysis. American Journal of Epidemiology. 2022;191(7):1323-1335. doi:10.1093/aje/kwac039
-
Taneri PE, Wehrli F, Roa-Díaz ZM, Itodo OA, Salvador D, Raeisi-Dehkordi H, et al. Association Between Ultra-Processed Food Intake and All-Cause Mortality: A Systematic Review and Meta-Analysis. American Journal of Epidemiology. 2022;191(7):1323-1335. doi:10.1093/aje/kwac039
-
Unknown. Ultra-processed food exposure and adverse health outcomes: umbrella review. BMJ; 2024. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10899807/
-
Lv J, Wei Y, Sun J, Shi Y, Liu F, Sun M, et al. Ultra-processed food consumption and metabolic disease risk: an umbrella review of systematic reviews with meta-analyses of observational studies. Frontiers in Nutrition. 2024;11. doi:10.3389/fnut.2024.1306310
-
Liliani L, Fatmawati F. Association Between Daily Alcohol Intake and Risk of All-Cause Mortality. The International Journal of Medical Science and Health Research. 2024;2(5):35-51. doi:10.70070/gx10jv51
-
Unknown. The relationship between alcohol consumption and health: J-shaped or less is more?. BMC Medicine; 2023. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-02911-w
-
World Health Organization. No level of alcohol consumption is safe for our health.. WHO Europe; 2023. https://www.who.int/europe/news-room/04-01-2023-no-level-of-alcohol-consumption-is-safe-for-our-health
-
NASEM. Review of Evidence on Alcohol and Health. 2025. https://www.ncbi.nlm.nih.gov/books/NBK614690/
-
Green CL, Lamming DW, Fontana L. Molecular mechanisms of dietary restriction promoting health and longevity. Nature Reviews Molecular Cell Biology. 2021;23(1):56-73. doi:10.1038/s41580-021-00411-4