Unit 1: Foundations of Longevity Coaching¶
Chapter 1.5: Scope of Practice & Medical Collaboration¶
[CHONK: 1-minute summary]
What you'll learn in this chapter:
- What scope of practice means and why it protects everyone: clients, you, and the profession
- The NBHWC scope boundaries: what you can and cannot do
- The Triangle of Care model: how clients, coaches, and physicians work together
- When and how to refer clients to medical providers
- Professional language that supports without prescribing
- Longevity-specific boundaries: supplements, biomarkers, medical interventions
The big idea: Scope of practice isn't about limiting what you can do. It's about keeping everyone safe. Longevity coaching intersects heavily with medicine, which makes clear boundaries essential. Every intervention, every conversation, every recommendation in this entire course must stay within these boundaries.
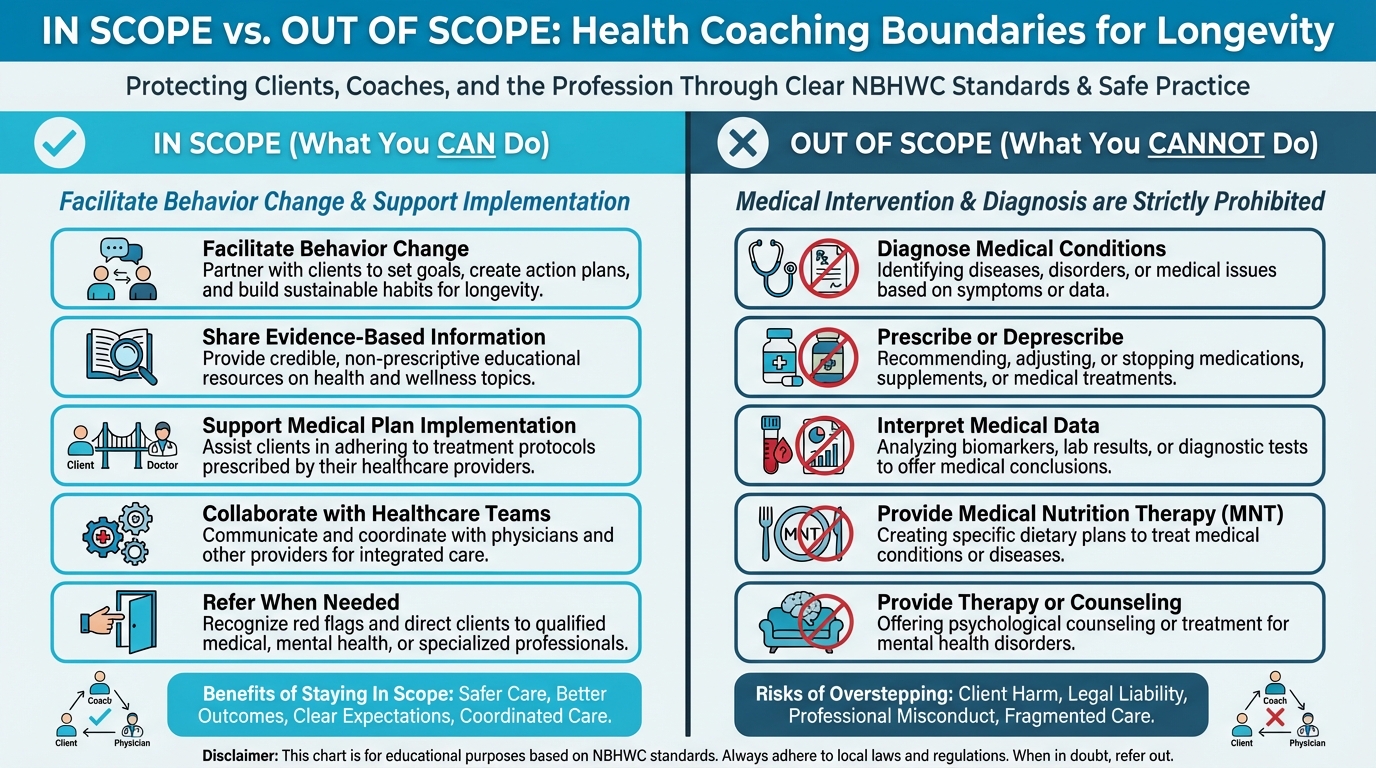
Figure: Clear boundaries visual
Introduction¶
Before we dive into interventions and strategies, we need to talk about boundaries. And if that sounds a little dry or legalistic, stick with us. This might be one of the most important chapters in the entire program.
Longevity coaching sits at a unique intersection where your clients will constantly ask questions that sound like they should have simple answers. They'll ask about hormones, supplements, biomarkers, and medical interventions. They'll bring you their lab results and want to know what the numbers mean. They'll ask whether they should take metformin, or try testosterone replacement, or start rapamycin.
These are medical questions. And if you answer them the way a doctor would—diagnosing conditions, interpreting test results, recommending treatments—you could be practicing medicine without a license. That's not just a technicality; it's illegal, and it could put your clients at real risk.
But here's what we want you to understand: knowing where the line is doesn't limit your ability to help. It actually makes you more helpful, because you can focus on what you do best—behavior change, habit building, lifestyle implementation—while making sure your clients get medical care from people who are credentialed to provide it. Think of it as professional clarity rather than professional limitation.
This chapter will show you exactly where that line is, and you might be surprised by how much room you have to work within it.
[CHONK: What Is Scope of Practice?]
What Is Scope of Practice?¶
Scope of practice is the legal and ethical boundary that defines what you can and cannot do as a health and wellness coach. Understanding it is one of the most important things you'll learn in this program.
Here's a simple way to think about it: a personal trainer can help you get stronger, but they can't diagnose a torn rotator cuff or prescribe physical therapy. A nutritionist can help you eat better, but they can't diagnose diabetes or prescribe medication. And a coach can help you change behaviors, navigate obstacles, and build sustainable habits. You can't diagnose conditions, interpret medical tests, or prescribe treatments.
Every profession has these boundaries, and they exist for good reasons: to protect clients from harm, to ensure practitioners have the right training for what they're doing, and to maintain the standards that make professions trustworthy.
The NBHWC Definition¶
The National Board for Health & Wellness Coaching (NBHWC) defines health and wellness coaches as accountability partners who facilitate client-led behavior change.¹ That phrase, "client-led", is important. We're not directors of care telling people what to do; we're partners helping them figure out what they want to do and how to actually do it.
What does that look like in practice? We help clients identify their own goals and values, explore their own motivations and barriers, create their own action plans, navigate obstacles when things get hard, and stay accountable to the commitments they've made to themselves. Everything we do is client-centered, which means our job is to facilitate their journey, not to prescribe the destination.
What Coaches CAN Do¶
Let's be clear about what you're absolutely allowed to do, because there's a lot here:
Share evidence-based information. You can educate clients about health topics, share what the research says, and provide resources that help them understand their options. You can explain what sleep hygiene is, discuss why strength training matters for longevity, or talk about how chronic stress affects the body. Education is absolutely in your wheelhouse.
Support implementation of treatment plans. When a physician prescribes a medication, you can help your client remember to take it consistently. When a dietitian creates a meal plan, you can help them actually follow it in their real life with their real schedule. You're the implementation partner, helping people do the things their healthcare team has recommended.
Collaborate with healthcare teams. With your client's consent, you can communicate with their physicians, dietitians, therapists, and other providers to coordinate care. This kind of collaboration often produces the best outcomes, because everyone is working from the same page.
Facilitate behavior change. This is your core function, the thing you're specifically trained to do. Goal-setting, habit building, accountability, motivational interviewing, helping people navigate the gap between knowing what to do and actually doing it. These are your tools, and they're powerful ones.
Refer when needs exceed coaching. When a client needs diagnosis, treatment, or specialized care that's beyond your scope, you refer them to the right provider. Knowing when to refer is a skill, and doing it well is part of being a great coach.
What Coaches CANNOT Do¶
Now for the other side, and this is where coaches sometimes get into trouble, often with the best of intentions:
Diagnose medical conditions. If a client says "I think I have diabetes" or "I think my thyroid is off," you cannot confirm or deny that. You can help them get to a doctor who can figure it out, but the diagnosis itself isn't yours to make.
Interpret medical data. You cannot tell clients what their lab results mean or whether their numbers are "normal" or "concerning." You can help them understand what different tests measure in general terms, but interpreting their specific results in a way that informs medical decisions? That requires medical training you don't have (and probably don't want. That's a lot of school).
Prescribe or deprescribe medications. You cannot recommend that clients start, stop, or change medications. Even if you've read all the research on metformin for longevity, you cannot tell a client they should take it. That's a physician's call.
Recommend supplements. This one surprises many coaches, but you cannot recommend specific supplements, brands, or dosages. You can educate about what the research says in general, but specific recommendations—"You should take vitamin D" or "Try this brand of fish oil"—require medical evaluation of that individual's needs.
Provide nutrition consultation or meal plans. You cannot create individualized meal plans or diagnose food allergies and intolerances. You can share general nutrition information and support behavior change around eating, but prescriptive nutrition requires a registered dietitian.
Provide exercise prescription. You cannot prescribe specific exercise programs. (If you're also a certified personal trainer, you can do this in that role, but you need to clearly separate your coaching hat from your training hat.)
Deliver psychological therapy. You cannot diagnose mental health conditions or provide therapy. You can absolutely support clients emotionally and help them develop coping skills, but there's a line between coaching support and therapeutic intervention, and you need to stay on the coaching side.
Why These Boundaries Exist¶
These boundaries might feel frustrating sometimes, especially when you're pretty sure you know the answer to a client's question. (We get it.) But they exist for genuinely important reasons:
Client safety. A coach who diagnoses conditions might delay proper medical care. A coach who recommends supplements might cause dangerous interactions with medications the client is taking. A coach who interprets lab results might miss something serious that a trained physician would catch. These aren't hypothetical risks. They happen.
Legal protection. Practicing medicine without a license is illegal everywhere, and the consequences can be serious: criminal charges, civil lawsuits, loss of your coaching credential. Staying in scope keeps you protected.
Professional integrity. When coaches overstep their boundaries, it damages the entire profession's reputation. It makes doctors less likely to collaborate with coaches, makes clients less sure they can trust us, and makes it harder for all of us to do good work.
The Reality: Many Coaches Overstep¶
Despite these clear boundaries, a lot of coaches still cross them. A 2025 study examining 560 health coach websites found that 29% recommended supplements, 17% sold supplements directly, and nearly a quarter of non-board-certified coaches were selling supplements.² That's concerning, both for the clients who might be harmed and for the profession as a whole.
Your job is to be different. Know where the lines are, stay inside them, and help your clients get complete care from the right providers.
| For DIY Learners |
|---|
| Applying this to yourself: Even when you're your own "client," scope of practice matters. The same boundaries that protect coaching clients protect you. Lifestyle changes—nutrition, exercise, sleep, stress—are yours to experiment with. But medical decisions (medications, hormones, interpreting lab values) belong with healthcare providers. Build your own "Triangle of Care" with providers you trust, and use this course to become a more informed, effective partner in your own healthcare. |
[CHONK: Coaching in Practice - "Just Tell Me What to Take"]
Coaching in Practice: "Just Tell Me What to Take"¶
The scenario: Kevin, 54, has been deep in longevity research online. He comes to your session with a list of supplements he's read about. "I've been researching NMN, resveratrol, and metformin. Just tell me which ones to take. You're the expert here."
What NOT to do:
❌ "Well, NMN has pretty good research behind it. I'd start with 500mg daily. Thorne makes a solid product."
Why this doesn't work: You've just recommended a specific supplement at a specific dose from a specific brand. That's prescribing, and it's outside your scope, even if the recommendation happens to be reasonable.
❌ "I can't tell you anything about supplements. That's not what I do."
Why this doesn't work: You've shut down the conversation without providing any value. Kevin will just find someone else who will give him recommendations, and that person might not be qualified either.
What TO do:
✅ Educate generally, acknowledge the interest, and redirect to appropriate providers while offering what you can help with.
Sample dialogue:
Kevin: "Just tell me which supplements to take. You're the expert."
Coach: "I appreciate that trust, Kevin, really. But I'm not actually the right expert for that specific question. Supplement recommendations need to come from someone who can look at your full health picture, your medications, your individual biochemistry. What I can do is different, but honestly? Probably more valuable."
Kevin: "So you can't help me at all with this?"
Coach: "I can absolutely help, just not by telling you what to take. What I can do is share what the research actually says about these compounds, help you think through what questions to ask your doctor, and help you implement the lifestyle changes that have much stronger evidence for longevity than any supplement. Those fundamentals often matter more than anything you could buy in a bottle."
Kevin: "Okay, so what does the research say?"
Coach: "NMN and resveratrol have shown some interesting results in animal studies, but the human data is still pretty limited. We just don't know yet whether they actually extend human lifespan. Metformin is a different story because it's a prescription medication, so that's definitely a conversation for your doctor, not me. The honest truth? The evidence for lifestyle factors—consistent exercise, good sleep, quality nutrition—is orders of magnitude stronger than for any supplement. Would you be interested in exploring what changes in those areas might give you the biggest return?"
Kevin: "I guess I assumed supplements were the shortcut."
Coach: "A lot of people do. The supplement industry is really good at marketing. But if you're serious about longevity, the fundamentals are where the real gains are. And those are exactly the things we can work on together."
Key takeaway: Educate about evidence, redirect to appropriate providers for specific recommendations, and emphasize what you can help with, which is actually quite a lot.
[CHONK: The Triangle of Care]
The Triangle of Care: Client, Coach, Physician¶
The Triangle of Care is Precision Nutrition's model for how clients, coaches, and physicians work together effectively. And understanding it will make you a better collaborator and a more valuable member of your clients' healthcare team.
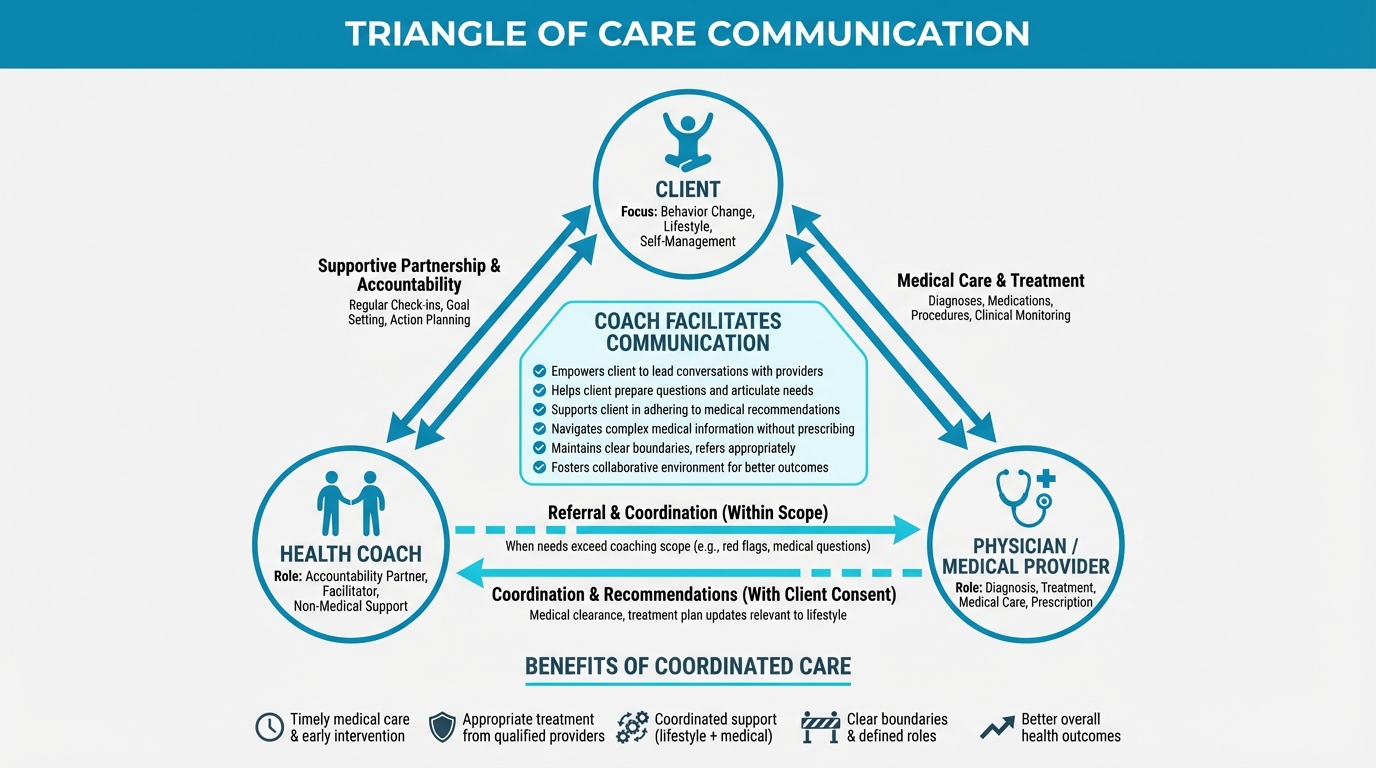
Figure: How coach facilitates provider communication
The Three Roles¶
The Client: The CEO
Think of the client as the CEO of their own health. They make the decisions, they own the outcomes, and they choose which direction to go. Your job isn't to replace the CEO. It's to support them in making good decisions and executing their vision effectively.
The Coach: The Project Manager
You're the project manager who helps the CEO actually get things done. You break big goals into manageable steps, identify obstacles and help find solutions, keep things on track, coordinate with other team members, and help navigate the inevitable challenges that come up along the way. Your focus is on lifestyle, habits, and execution: the day-to-day work of actually living differently.
The Physician: The Medical Expert
The physician handles the medical side: diagnosing conditions, ordering and interpreting tests, prescribing treatments, and managing medical risk. Their focus is on diagnosis, treatment, and risk management: things that require medical training and credentials.
How They Work Together¶
When the Triangle of Care is working well, it looks something like this:
The client decides what they want. "I want to optimize my health for longevity" or "I want to reduce my risk of the diseases that run in my family."
The physician determines what's medically appropriate. "Based on your labs, here's what I'm seeing and here's what I recommend from a medical standpoint."
The coach helps implement lifestyle changes. "Your physician flagged some areas of concern. Let's explore what lifestyle changes you're willing and able to make, and figure out how to actually fit them into your life."
Everyone stays in their lane, but everyone is rowing in the same direction.
Evidence for Collaborative Care¶
The research on collaborative care models is compelling: when coaches work alongside medical providers rather than in isolation, clients get meaningfully better outcomes.
A 2023 meta-analysis of 30 studies found that health coaching significantly improved quality of life, self-efficacy, and depressive symptoms compared to usual medical care alone.³ A 2017 VA synthesis found that adding health coaching reduced HbA1c (a key diabetes marker) and improved physical activity and dietary habits.⁴ And a 2020 study found that integrated care teams including health coaches reduced total healthcare costs by 12.6% while improving diabetes control, compared to a 51.7% increase in costs for usual care.⁵
The evidence is clear: you add real value when you work as part of a team. But that value depends on everyone understanding their role.
[CHONK: Coaching in Practice - "My Doctor Doesn't Listen"]
Coaching in Practice: "My Doctor Doesn't Listen"¶
The scenario: Sandra, 61, is frustrated with her healthcare experience. "My doctor won't prescribe testosterone. I've read it's important for women's health and longevity too, but he just dismisses me. Can you write me a letter supporting my case, or something like that?"
What NOT to do:
❌ "Your doctor should definitely consider testosterone for you. Here's some research you can show him to change his mind."
Why this doesn't work: You're undermining the physician's medical judgment and implying that a specific treatment is right for this client, which isn't your call to make.
❌ "I really can't get involved in your medical care. That's strictly between you and your doctor."
Why this doesn't work: You've abandoned her at a moment when she's feeling unheard and frustrated. She came to you for support, and you've essentially said "not my problem."
What TO do:
✅ Validate the frustration, support her advocacy, and help her navigate the system, without directing medical decisions.
Sample dialogue:
Sandra: "My doctor won't prescribe testosterone. Can you write me a letter or something?"
Coach: "I can really hear how frustrating this is. Feeling dismissed when you're trying to advocate for your own health is genuinely awful. Unfortunately, writing a letter that recommends a specific treatment isn't something I can do. That would be stepping into medical territory that's outside my scope."
Sandra: "So there's nothing you can do to help?"
Coach: "Actually, there's quite a bit I can help with. Just in a different way. What if we worked together on preparing for your next appointment? We could organize your symptoms, the questions you want to ask, the research you've found. Sometimes going in with a clear, organized case changes how those conversations go."
Sandra: "He just doesn't seem interested in longevity medicine at all."
Coach: "You might be right about that. Not every physician has deep familiarity with this space. One option worth considering: you could ask for a referral to an endocrinologist, or seek out a physician who specializes in hormone optimization. A second opinion is completely reasonable when you feel like your concerns aren't being heard."
Sandra: "I hadn't really thought about finding a different doctor."
Coach: "You're absolutely allowed to advocate for yourself, and part of that advocacy can be finding a provider who takes your concerns seriously. I can't tell you what treatment you should or shouldn't have. That's a medical decision. But I can support you in finding the right care team and preparing to have productive conversations with them."
Key takeaway: Support client advocacy without directing medical decisions. Help them navigate the healthcare system effectively, but don't try to influence what treatment they receive.
[CHONK: When to Refer]
When to Refer: Red Flags and Decision Trees¶
One of your most important skills as a coach is knowing when to refer, when a client needs something that's beyond what coaching can provide. Refer too early and you might interrupt helpful work; refer too late and you might miss something serious. The key is having clear criteria that help you make the right call.
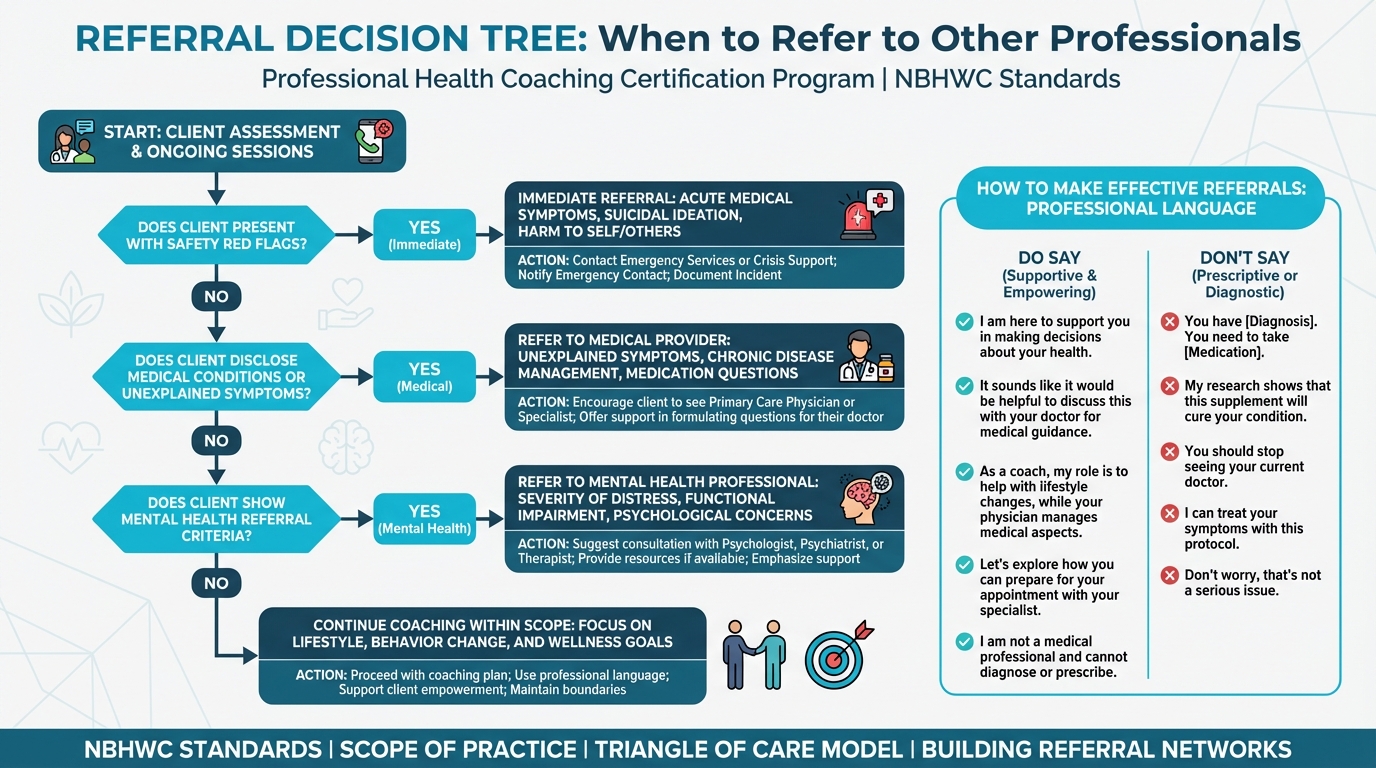
Figure: When to refer to other professionals
Safety Red Flags: Immediate Referral¶
Some situations require immediate action: no hesitation, no "let's see how it goes." These are non-negotiable:
Suicidal ideation or intent to harm. If a client expresses thoughts of suicide, self-harm, or harming others, you stop coaching immediately and refer to emergency services or a crisis hotline. This takes priority over everything else, and you don't continue coaching until they've received appropriate professional care.
Acute medical symptoms. Chest pain or pressure, severe shortness of breath, sudden severe headache, loss of consciousness, signs of stroke (sudden weakness, confusion, speech difficulties). These are emergencies. Refer to emergency care immediately.
Severe mental health symptoms. Severe depression that's preventing normal functioning, psychotic symptoms like hallucinations or delusions, severe anxiety that's making daily life impossible, substance use that's causing significant harm. These need immediate mental health intervention.
Medical Conditions Requiring Referral¶
Beyond emergencies, certain situations need physician evaluation:
Unexplained symptoms like weight changes without clear cause, persistent fatigue that doesn't respond to lifestyle changes, chronic pain, ongoing digestive issues, or skin changes that concern you.
Suspected eating disorders: any pattern of restrictive eating, binge eating, purging, body image distortion, or obsessive thoughts about food and weight warrants referral to eating disorder specialists.
Medication questions: anything about starting, stopping, or changing medications, including concerns about side effects or interactions.
Poorly controlled chronic conditions: diabetes with blood sugars that aren't responding to lifestyle changes, hypertension that remains elevated, heart disease with new or worsening symptoms.
Mental Health Referral Criteria¶
Mental health is an area where coaches often wonder about boundaries. Here's a framework:
Immediate referral (safety): Suicidal or homicidal ideation, severe self-harm.
Urgent referral (within days): Severe depression or anxiety with significant functional impairment, psychotic symptoms, substance use that's causing harm.
Routine referral (within weeks): Moderate depression or anxiety that's persisting, trauma symptoms, grief that's not resolving, relationship issues that are significantly affecting mental health.
You can use brief screening tools like the PHQ-2 to help identify clients who need mental health assessment. A score of 3 or higher suggests further evaluation by a mental health provider is warranted.⁶
The Decision Tree¶
When you're unsure whether to refer, work through this sequence:
Step 1: Is this a safety issue? If yes, refer immediately to emergency services. Don't continue coaching until it's resolved.
Step 2: Is this a medical question? If yes, refer to the appropriate medical provider. You can continue coaching on lifestyle factors, but the medical question needs medical expertise.
Step 3: Is this within my coaching scope? If yes, continue coaching. If you're not sure, move to step 4.
Step 4: When in doubt, refer. It's always better to refer too early than too late. A good referral helps your client; a missed referral could harm them.
Making Referrals Effectively¶
How you make a referral matters as much as whether you make one:
Explain why you're referring. "This is a medical question that needs a physician's expertise. I can absolutely help you implement lifestyle changes, but the medical decision itself needs to come from your doctor."
Normalize the referral. Don't make it sound like something has gone wrong. "This is exactly the kind of situation where working with a specialist makes sense. You'll get the medical guidance you need, and I'll keep supporting the lifestyle piece."
Be specific. Don't just say "see a doctor." Say "I'd recommend seeing an endocrinologist who specializes in hormone health" or "A registered dietitian could create a meal plan tailored to your specific needs."
Support the transition. Help clients prepare for the appointment. What questions to ask, what information to bring, what to expect.
Follow up. After the referral, check back: "How did your appointment go? What did they recommend? How can I help you implement what they suggested?"
[CHONK: Coaching in Practice - Referral Resistance]
Coaching in Practice: "I Don't Want to See a Doctor"¶
The scenario: Thomas, 58, has mentioned chest tightness during exercise several times over the past few weeks. When you suggest he should see a cardiologist before continuing with his exercise program, he pushes back: "I'm fine, really. It's just stress or something. I don't need to see a doctor about it."
What NOT to do:
❌ "Okay, if you're sure. Let's just back off the intensity a bit and see if that helps."
Why this doesn't work: Chest tightness during exercise is a red flag that could indicate something serious. You can't just work around it because he doesn't want to hear it.
❌ "I'm not going to work with you until you see a doctor. Period."
Why this doesn't work: While your concern is valid, ultimatums often backfire. He might just stop mentioning symptoms to you, which is worse.
What TO do:
✅ Be direct about your concern, explore what's behind the resistance, and maintain a firm but collaborative boundary.
Sample dialogue:
Coach: "Thomas, I have to be really direct with you about something. Chest tightness during exercise is something that needs medical evaluation. This isn't optional from my perspective."
Thomas: "It's really not that bad. I'm sure it's just stress."
Coach: "It might be stress, you're right. But here's what I know: chest symptoms during exertion can sometimes indicate heart issues that are very treatable if you catch them early, and potentially serious if you don't. I'm not qualified to tell you which situation you're in. And honestly, neither are you."
Thomas: "Doctors always find something wrong. I don't want to hear that I can't exercise anymore."
Coach: "Ah, okay, that's what you're worried about. That makes sense, actually. But think about it this way: if the cardiologist finds nothing wrong, you get peace of mind and we can keep training with confidence. If they do find something, you're catching it early when it's most treatable. Either way, you're in a better position than you are right now, wondering."
Thomas: "I'll think about it."
Coach: "I need a bit more than that, Thomas. Here's where I have to draw a line: I can't design exercise programs for someone who has unexplained chest symptoms. That would be putting you at risk and taking me way outside my scope. Get cleared by a cardiologist, and we can move forward with a program I feel good about. Does that make sense?"
Thomas: "When you put it that way... yeah, okay. I'll make an appointment."
Key takeaway: Some referrals aren't optional. Be direct and caring, explore the resistance to understand what's really going on, but maintain the boundary when safety is at stake.
[CHONK: Professional Language]
Professional Language: Supporting Without Prescribing¶
The words you choose matter more than you might think. The difference between staying in scope and overstepping often comes down to how you phrase things. Supporting language helps clients explore and decide for themselves, while prescribing language tells them what to do.
The Core Distinction¶
Prescribing language (avoid):
- "You should take vitamin D."
- "You need to exercise more."
- "You must cut out sugar."
Supporting language (use):
- "Some research suggests vitamin D might be helpful for certain people. Have you talked with your doctor about whether it makes sense for you?"
- "What kind of movement feels realistic for your life right now?"
- "How do you want to approach the sugar question?"
Notice the difference: prescribing language makes the decision for the client, while supporting language helps them think through the decision themselves.
What to Say: Supplements¶
DON'T say:
- "You should take this supplement."
- "I recommend vitamin D for you specifically."
- "Take 5,000 IU daily."
DO say:
- "Some research suggests vitamin D might support bone health and immune function. Have you discussed supplementation with your physician?"
- "If you're interested in supplements, a registered dietitian or your doctor can assess your specific needs and make recommendations based on your individual situation."
- "I can share what the research says about different supplements, but specific recommendations really need to come from someone who can look at your full health picture."
What to Say: Biomarkers¶
DON'T say:
- "Your HbA1c is too high."
- "Your testosterone is low for your age."
- "These numbers are concerning."
DO say:
- "I see you have your HbA1c results here. Have you had a chance to discuss what these mean with your physician?"
- "Testosterone levels can vary a lot between individuals. What did your doctor say about your results?"
- "I can help you understand what these different tests measure, but interpreting your specific results in terms of what they mean for your health, that requires medical expertise I don't have."
What to Say: Medical Interventions¶
DON'T say:
- "You should try metformin for longevity."
- "I think hormone replacement therapy would help you."
- "You need this intervention."
DO say:
- "Metformin is a prescription medication that some people use for longevity. Have you discussed this possibility with your physician?"
- "Hormone replacement is a medical decision that involves weighing risks and benefits for your specific situation. What has your doctor said about your options?"
- "I can help you think through the lifestyle factors and prepare good questions for your medical team, but decisions about medical interventions really need to come from them."
Setting Boundaries Explicitly¶
Sometimes you need to be direct about what you can and cannot do:
When clients ask you to diagnose: "I'm not qualified to diagnose medical conditions. That requires evaluation by a physician. What I can do is help you prepare for that conversation and think through what questions you want to ask."
When clients ask you to prescribe: "I can't make medical recommendations; that's outside my scope as a coach. But I can help you understand your options and prepare for productive conversations with your healthcare team."
When clients push: "I understand you're looking for answers, and I wish I could give you a simple one. But this is really a medical question, and giving you a medical answer would be stepping outside what I'm trained and credentialed to do. What I can do is help with the lifestyle side, and that's honestly where a lot of the action is anyway."
[CHONK: Longevity-Specific Boundaries]
Longevity-Specific Scope Considerations¶
Longevity coaching has some unique scope challenges because the field sits right at the intersection of lifestyle and medicine. Here's how to navigate the most common situations.
Supplements: Education vs. Recommendation¶
What you CAN do:
- Educate about what supplements are and how they're regulated (spoiler: not very strictly)
- Share what the research says in general terms: what's promising, what's overhyped, what we don't know yet
- Help clients prepare thoughtful questions for their physician or dietitian
- Support lifestyle changes that might reduce the need for supplementation in the first place
What you CANNOT do:
- Recommend specific supplements, brands, or dosages for individual clients
- Diagnose nutrient deficiencies
- Assess whether supplements might interact with a client's medications
- Sell supplements or receive commissions from supplement sales
Why this matters: The supplement industry is lightly regulated: products don't need FDA approval before they're sold, quality varies enormously between brands, and interactions with medications are common but often not well-studied. That's exactly why specific recommendations need to come from someone with medical training who can evaluate an individual's full situation.
Biomarkers: Context vs. Interpretation¶
What you CAN do:
- Help clients understand what different biomarkers measure in general terms
- Support them in preparing for medical appointments where their results will be interpreted
- Help them implement lifestyle changes that might improve their markers over time
- Educate about the limitations and nuances of biomarker testing
What you CANNOT do:
- Interpret specific biomarker results for clients ("Your numbers look concerning")
- Diagnose conditions based on biomarkers
- Recommend interventions based on what you see in their results
- Order biomarker tests
The key distinction: Explaining what HbA1c measures (average blood sugar over time) is education. Telling a client "Your HbA1c of 6.2 means you have prediabetes and need to make changes" is interpretation that crosses into medical territory.
Medical Interventions: Support vs. Prescribe¶
What you CAN do:
- Educate about what various longevity interventions are and what the evidence says about them
- Help clients prepare for medical appointments where they'll discuss these options
- Support adherence to interventions their physician has prescribed
- Help them implement lifestyle changes alongside medical treatment
What you CANNOT do:
- Recommend medical interventions
- Diagnose conditions that might warrant interventions
- Prescribe or adjust medications
- Second-guess medical decisions their physician has made
Common longevity interventions like hormone replacement therapy, metformin, and rapamycin are prescription medications that require physician evaluation, ongoing monitoring, and medical management. You can be a valuable support partner, but the medical decisions aren't yours to make.
[CHONK: Building Referral Networks]
Building Referral Networks¶
One of the most valuable things you can do for your practice, and for your clients, is build a network of trusted providers you can refer to with confidence.
Types of Providers to Include¶
Primary care physicians who understand preventive medicine and are open to lifestyle interventions as a first-line approach.
Specialists based on your client population: endocrinologists for hormone and metabolic issues, cardiologists for cardiovascular concerns, registered dietitians for nutrition therapy, mental health providers (therapists, psychologists, psychiatrists), physical therapists for movement issues, and if you work with longevity-focused clients, physicians who specialize in longevity medicine.
How to Find Good Providers¶
Ask colleagues and other wellness professionals who they trust and refer to, and check professional directories like the American College of Lifestyle Medicine or Institute for Functional Medicine. You can also use insurance network directories to find providers your clients can actually afford to see and attend local health and wellness networking events to expand your connections. Finally, ask clients who've had good experiences for recommendations (with their permission to share).
Building Relationships¶
Once you've identified promising providers, reach out to introduce yourself. Explain what you do as a coach, how you stay within your scope, and how you'd like to collaborate. Ask about their referral preferences: how they like to receive referrals, what information is helpful to include. Follow up after you send them clients to close the loop and strengthen the relationship.
Good provider relationships are professional, not personal. You're building a network, not a social circle. Keep it focused on serving clients well.
The Bottom Line: Why All of This Protects Everyone¶
We've covered a lot of ground on boundaries, and it might feel like a lot of rules. But here's the reframe: these boundaries aren't limitations on what you can do. They're the foundation that makes everything else possible.
When you stay in scope, your clients get safer, more coordinated care. They get medical expertise from people trained to provide it, and behavior change support from someone specifically skilled in that work. They don't fall through the cracks between providers, and they don't get medical advice from someone who isn't qualified to give it.
When you stay in scope, you get legal protection and professional credibility. You're practicing within your credentials, which means physicians are more likely to collaborate with you, clients are more likely to trust you, and you're not carrying risk you shouldn't be carrying.
And here's the mindset shift that makes all of this feel right: staying in scope isn't about what you know. It's about what you're credentialed to do. You might know quite a lot about supplements or hormones or longevity interventions. (We hope you will, after this course!) But knowing something isn't the same as being credentialed to make decisions based on that knowledge. A brilliant software engineer might know how to rewire a house, but they're not a licensed electrician.
Your scope is a feature, not a limitation. It lets you focus on what you do best, and it ensures your clients get complete care from the right people.
Study Guide Questions¶
-
What is scope of practice, and why does it matter specifically for longevity coaches?
-
According to the NBHWC, what are three things coaches CAN do and three things they CANNOT do?
-
Explain the Triangle of Care model. What are the three roles, and how do they work together?
-
What are safety red flags that require immediate referral, no exceptions?
-
How should coaches handle questions about supplements? What can you say, and what crosses the line?
-
A client brings lab results and asks what their numbers mean. How do you respond while staying in scope?
-
A client is frustrated that their doctor won't prescribe a treatment they've read about. How do you support them without directing medical decisions?
-
When should you refer for mental health concerns? What's the difference between immediate, urgent, and routine referrals?
-
What's the difference between supporting language and prescribing language? Give examples of each.
-
How do the scope boundaries covered in this chapter apply to everything else in this course?
Self-reflection questions:
-
If you're applying this course to your own life, who are the healthcare providers on your personal "Triangle of Care"? Do you have a primary care physician you trust? Are there specialists (cardiologist, endocrinologist, etc.) you might need to add to your team?
-
Think about a health question you've been curious about. Is it something you can address through lifestyle changes yourself, or something you should discuss with a healthcare provider?
[CHONK: Works Cited]
Deep Dives¶
Want to go deeper? These supplemental articles explore key topics from this chapter in more detail.
- Building Your Referral Network. How to connect with local providers
References¶
-
National Board for Health & Wellness Coaching. Health & Wellness Coach Scope of Practice. 2023. https://nbhwc.org/scope-of-practice/
-
Suleta K, Davis JM. An Examination of Health Coaching as a Developing Profession. HCA Healthcare Journal of Medicine. 2025;6(2). doi:10.36518/2689-0216.1919
-
Boehmer KR, Álvarez-Villalobos NA, Barakat S, et al. The impact of health and wellness coaching on patient-important outcomes in chronic illness care: A systematic review and meta-analysis. Patient Education and Counseling. 2023;117:107975. doi:10.1016/j.pec.2023.107975
-
Gierisch JM, et al. The effectiveness of health coaching. US Department of Veterans Affairs Evidence Synthesis Program. 2017. https://www.ncbi.nlm.nih.gov/books/NBK487705/
-
Fortmann AL, Walker C, Barger K, et al. Care Team Integration in Primary Care Improves One-Year Clinical and Financial Outcomes in Diabetes. Population Health Management. 2020;23(6):467-475. doi:10.1089/pop.2019.0103
-
Family-Centered Coaching Toolkit. Referring clients for mental health services. 2011. https://www.familycenteredcoaching.org/
Chapter 1.5 complete. Proceed to Chapter 1.6: The Coaching Process.