Unit 1: Foundations of Longevity Coaching¶
Chapter 1.4: Assessment & Biomarkers¶
[CHONK: 1-minute summary]
What you'll learn in this chapter:
- Which tests matter for longevity tracking (and which are optional)
- How to interpret results within coaching scope: what you can say, what needs referral
- How to conduct Deep Health assessments across all six dimensions
- How to use assessment data to motivate clients and guide coaching conversations
The big idea: You can't coach longevity without measuring it. But assessment isn't just about collecting numbers. It's about knowing what those numbers mean, staying within your scope, and using data to personalize your approach. This chapter teaches you the essential biomarkers, functional tests, and subjective assessments that form the foundation of evidence-based longevity coaching.
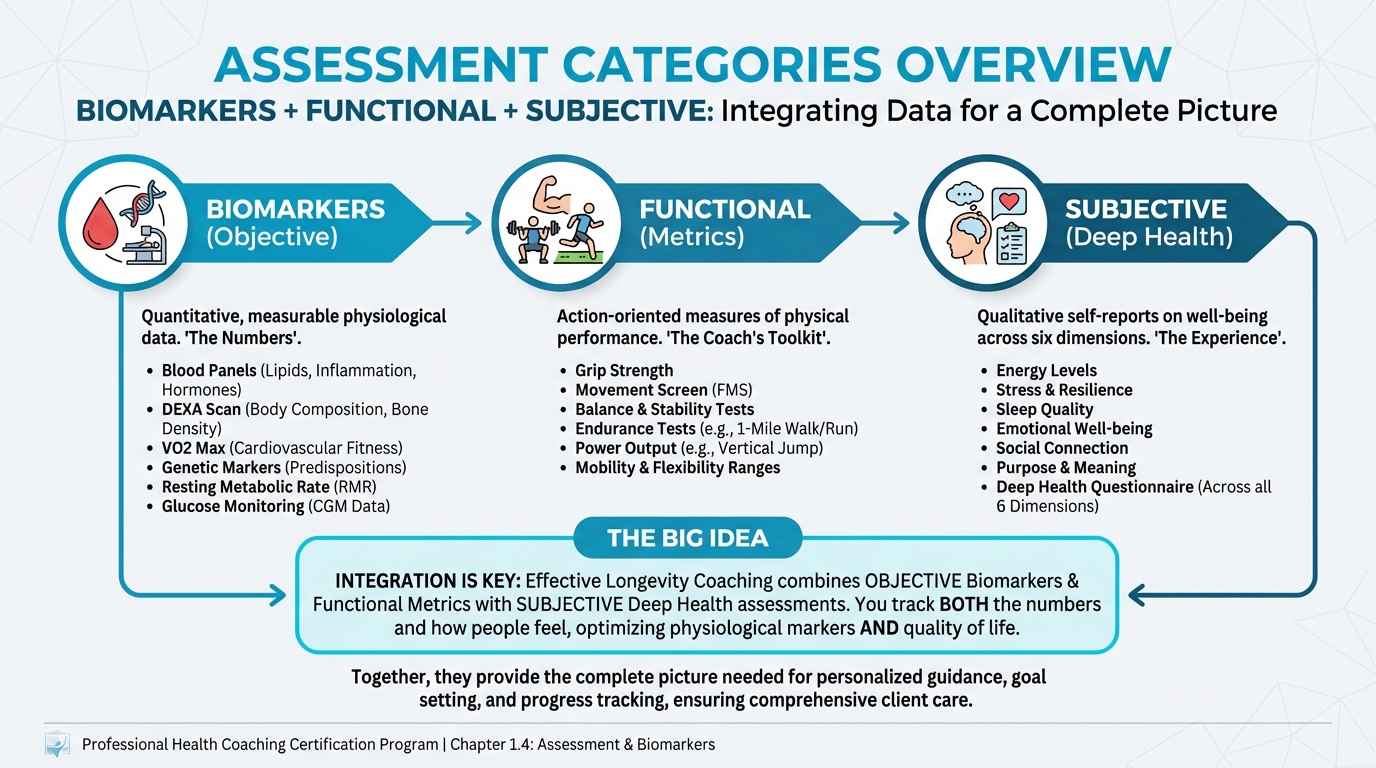
Figure: Biomarkers + Functional + Subjective
Introduction¶
Assessment is the foundation of effective longevity coaching. Without measurement, you're guessing. With measurement, you know where clients are starting, whether interventions are working, and what to prioritize.
But here's what new coaches often miss: assessment isn't just about tests and numbers. It's about understanding what those numbers mean, and equally important, what they don't mean. It's about knowing what you can say to clients versus what requires a doctor.
This chapter covers:
1. Functional metrics: the tests you can help clients improve (VO2 max, grip strength, movement tests)
2. Imaging and blood panels: what they measure and how to discuss results in scope
3. Deep Health assessments: the subjective side that objective tests miss
4. Putting it together: creating practical assessment protocols for real clients
One principle guides everything: screen, don't diagnose. You can recommend tests, discuss trends, and explain what numbers generally mean. You cannot diagnose conditions or prescribe treatments. That line keeps you in scope and protects your clients.
[CHONK: Functional Metrics - The Tests You Can Actually Improve]
Functional Metrics — The Coach's Power Zone¶
Functional metrics are special: they predict longevity AND you can directly help clients improve them, which means they're not just assessment tools but intervention targets.
VO2 Max: The Strongest Mortality Predictor¶
VO2 max measures your body's maximum ability to use oxygen during exercise. It's the single strongest predictor of all-cause mortality among all biomarkers.¹
The numbers are striking: people with the highest cardiorespiratory fitness have approximately 53% lower all-cause mortality compared to those with the lowest fitness.² Each 1-MET increase associates with 11-17% lower mortality risk.³
Target: The Longevity Protocol recommends 35+ mL/kg/min as a longevity goal. This is achievable for most people with consistent aerobic training.
How to measure:
- Lab testing: Direct measurement with respiratory gas analysis (gold standard, expensive)
- Field tests: Cooper 12-minute run, step tests (accessible, valid for tracking trends)
What coaches can say: "Higher VO2 max is associated with longer life. The research is clear: fit people live longer. We can improve yours through consistent aerobic training: Zone 2 work most days, plus some higher-intensity intervals."
Refer when: Client experiences chest pain, dizziness, or abnormal symptoms during testing.
Grip Strength: A Window into Overall Health¶
Grip strength isn't just about your hands; it's a proxy for overall muscle function throughout the body.
Lower grip strength consistently predicts higher mortality. People in the highest tertile have 59-62% lower mortality risk compared to the lowest tertile.⁴ Each 1-kg increase in grip strength associates with 2-10% reduced mortality risk depending on population.⁵
Thresholds: The EWGSOP2 guidelines define probable sarcopenia at <27 kg for men and <16 kg for women.
Tracking target: Weekly grip testing with a goal of 70+ pounds as a strength proxy.
What coaches can say: "Grip strength reflects your overall muscle function. Research shows weaker grip predicts higher mortality. If your grip is low, that tells us to focus on whole-body strength training, not just your hands."
Refer when: Grip dramatically below thresholds, especially with other signs of muscle loss (difficulty rising from chairs, unexplained weight loss).
Movement Tests: Simple, Free, Highly Predictive¶
These tests require no equipment and predict mortality surprisingly well.
Sit-to-rise test: Start seated on the floor, rise to standing without using hands or knees. Each support point used subtracts from score.
- Lower scores predict higher mortality. The lowest scores showed 5.44 times higher mortality risk over 6.3 years⁶
- Each 1-point improvement associates with ~21% better survival
Timed Up-and-Go (TUG): Rise from chair, walk 3 meters, turn, walk back, sit down.
- ≥9 seconds indicates higher risk, approximately 2.66 times higher mortality⁷
- Each additional second associates with ~5% increased mortality
Gait speed: Simple walking speed.
- Each 0.1 m/s slower associates with 12% higher mortality⁸
| For DIY Learners |
|---|
| Applying this to yourself: Try the sit-to-rise test right now. Sit on the floor, then stand up using as little support as possible. Score 5 points for sitting and 5 for rising, subtracting 1 point each time you use a hand, knee, forearm, or side of leg for support. A score below 8 suggests you'd benefit from focused mobility and strength work. This isn't about judgment—it's about knowing where you are so you can improve. |
One-legged stance: Balance on one leg for 10 seconds.
- Inability to complete predicts 1.84 times higher mortality over 7 years⁹
What coaches can say: "These tests show how well your body moves and functions. People who score well live longer. The good news: strength training, balance work, and mobility exercises all improve these scores."
Refer when: Client can't safely attempt tests (high fall risk, severe balance issues).
[CHONK: Coaching in Practice - Assessment Resistance]
Coaching in Practice: "I Don't Want to Know My Numbers"¶
The scenario: Patricia, 54, wants to "feel better" but resists any testing. "I already know I'm out of shape. Why do I need a test to tell me that?"
What NOT to do:
❌ "Testing is essential for longevity coaching. We really need baseline data."
Why it doesn't work: You've made it about your needs, not hers. She'll dig in deeper.
What TO do:
✅ Acknowledge the resistance, then reframe assessment as empowerment.
Sample dialogue:
Coach: "I hear that. You're worried about seeing numbers you won't like?"
Patricia: "Exactly. I'll just feel worse about myself."
Coach: "That makes sense. But here's what I've noticed: people who avoid testing are usually guessing, and often guessing wrong. You 'think' you're out of shape, but you don't actually know which parts of your health need attention most."
Patricia: "I mean... I know my cardio is bad."
Coach: "Maybe. Or maybe your cardio is better than you think and it's actually strength we should focus on. Or balance. Testing isn't about making you feel bad. It's about knowing where to focus. What if we started with something simple? Grip strength takes 30 seconds. Would you be willing to try that one thing?"
Patricia: "I guess grip strength doesn't sound too scary."
Coach: "Perfect. Let's start there. You might be pleasantly surprised."
Key takeaway: Start with the least threatening test. Build trust before full assessment.
[CHONK: Imaging and Blood Panels]
[CHONK: Imaging and Blood Panels]
Imaging Tests¶
DEXA Scans: Body Composition and Bone Health¶
DEXA measures three things that matter for longevity:
- Bone mineral density (BMD). Fracture risk indicator
- Body composition. Lean mass, fat mass, body fat percentage
- Visceral adipose tissue (VAT). The dangerous fat around organs
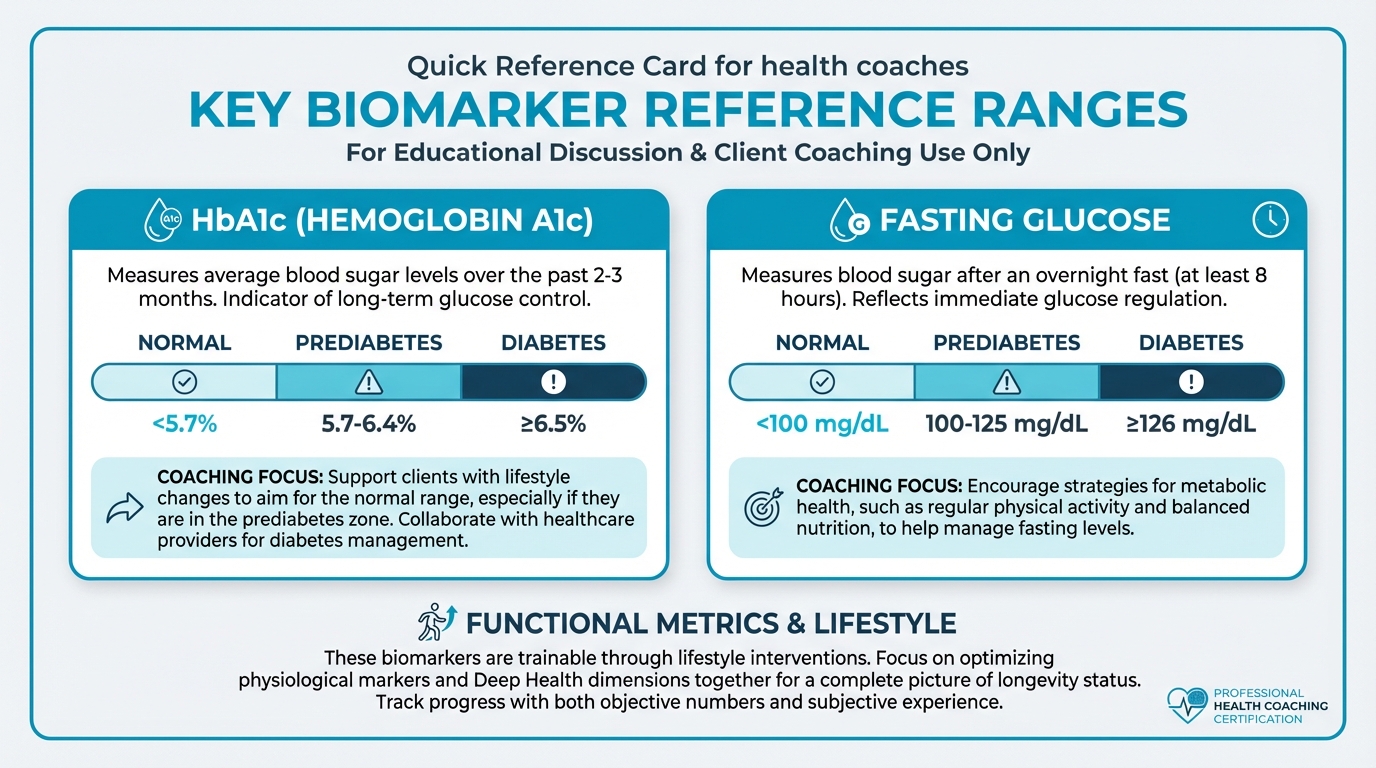
Figure: Normal/optimal ranges for key markers
What coaches can say about body composition: "Your DEXA shows how much muscle and fat you have, and where the fat is stored. Higher muscle mass and lower visceral fat associate with better longevity. We'll use this as a baseline to track changes."
What coaches can say about bone density: "Your DEXA includes bone density measurements. Your doctor should interpret the T-score for any medical diagnosis. I can tell you that strength training and adequate protein/calcium support bone health."
T-scores (for reference, not diagnosis):
- Normal: ≥ -1.0
- Osteopenia: -1.0 to -2.5
- Osteoporosis: ≤ -2.5
Refer when: T-score ≤ -2.5, rapid bone density decline, or any questions about medical implications.
Frequency: Annually for body composition; every 2-3 years for bone density.
Blood Panels¶
Blood panels provide a window into metabolic health, inflammation, and cardiovascular risk. A critical reminder: you cannot independently interpret medical lab results; you can discuss trends, lifestyle connections, and general education, but medical interpretation belongs to physicians.
Metabolic Markers¶
HbA1c: Average blood sugar over 2-3 months
- Normal: <5.7%
- Prediabetes: 5.7-6.4%
- Diabetes: ≥6.5%
Fasting glucose: Blood sugar after an overnight fast
- Normal: <100 mg/dL
- Prediabetes: 100-125 mg/dL
- Diabetes: ≥126 mg/dL
What coaches can say: "These markers reflect blood sugar control, and higher values suggest insulin resistance, which means your body isn't responding to insulin efficiently. We can address this through nutrition and exercise, both of which improve insulin sensitivity."
Refer when: HbA1c ≥6.5% or fasting glucose ≥126 mg/dL (diabetes range).
Inflammatory Markers¶
hsCRP: High-sensitivity C-reactive protein measures chronic inflammation
- Low risk: <1 mg/L
- Average risk: 1-3 mg/L
- High risk: >3 mg/L
What coaches can say: "Higher inflammation is associated with accelerated aging. Lifestyle changes—exercise, anti-inflammatory nutrition, stress management, quality sleep—can help reduce chronic inflammation."
Refer when: Very high values (>10 mg/L) may indicate acute infection or autoimmune conditions.
Lipids¶
ApoB: Number of atherogenic particles (superior cardiovascular risk marker)
Traditional panel: Total cholesterol, LDL, HDL, triglycerides
What coaches can say: "These markers relate to cardiovascular risk. Lifestyle changes—regular exercise, Mediterranean-style eating, maintaining healthy weight—can positively impact these numbers."
Refer when: Very elevated values, need for medication decisions, concerning trends despite lifestyle changes.
Hormones: Medical Territory¶
Hormone panels (testosterone, estrogen, thyroid) require physician interpretation. Coaches should not interpret hormone results or recommend hormone optimization.
What coaches can say: "Hormone levels change with age. If you're experiencing symptoms like fatigue, mood changes, or low energy, discuss hormone testing with your doctor. I can support your overall health through lifestyle—exercise, sleep, stress management—which all influence hormone function."
[CHONK: Coaching in Practice - Blood Work Discussion]
Coaching in Practice: Discussing Blood Results¶
The scenario: Marcus, 51, brings his lab results. HbA1c is 6.2% (prediabetic), hsCRP is 3.8 (elevated), ApoB is 115 (moderately elevated). He wants you to "explain what this all means."
What NOT to do:
❌ "Your HbA1c of 6.2% means you have prediabetes. Your inflammation is concerning. We need to address this immediately."
Why it doesn't work: You've just diagnosed him ("you have prediabetes") and created alarm without actionability.
What TO do:
✅ Educate generally, emphasize lifestyle connections, include referral language.
Sample dialogue:
Coach: "Thanks for sharing these. Let me walk you through what these markers generally indicate, and then we'll talk about what you should discuss with your doctor.
Your HbA1c is 6.2%. This marker reflects average blood sugar over the past few months. Values between 5.7 and 6.4 are considered the 'prediabetes' range, meaning blood sugar control isn't as efficient as it could be. The good news? This responds really well to lifestyle changes."
Marcus: "So I have prediabetes?"
Coach: "Your doctor would make that determination. What I can tell you is that these values are in a range where nutrition and exercise make a real difference. People often see significant improvement with consistent changes.
Your hsCRP is 3.8, which suggests some chronic inflammation. Again, lifestyle factors—exercise, anti-inflammatory foods, sleep, stress management—can help lower this.
Here's what I recommend: Schedule a follow-up with your doctor to review these results in context of your full health picture. Then let's build a plan together. What would you like to focus on first: the nutrition side or the exercise side?"
Key takeaway: Educate without diagnosing, always include "discuss with your doctor," and focus on actionable lifestyle interventions.
Deep Health Assessments — What Numbers Miss¶
[CHONK: Deep Health Assessment]
Deep Health Assessments — What Numbers Miss¶
Objective tests miss something important: how people feel. Someone with perfect blood work might be exhausted and miserable, while someone with mediocre biomarkers might feel great, which is why you need both objective and subjective data.
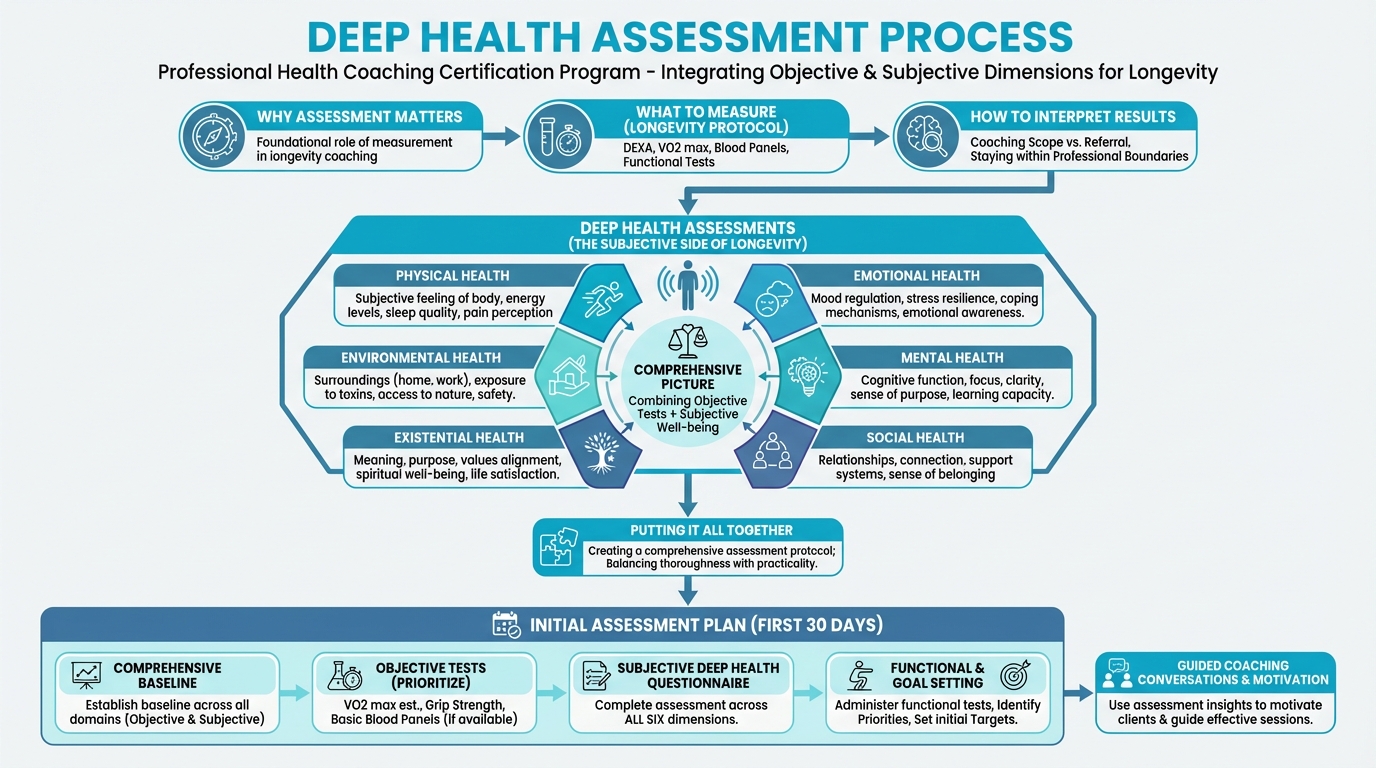
Figure: How to conduct 6-dimension assessment
The Six Dimensions Applied¶
For each dimension, assess current state, challenges, strengths, and connections to other dimensions.
Physical: Energy levels, sleep quality, pain, physical function, recovery
- "On a scale of 1-10, how would you rate your energy most days?"
- "Do you wake up feeling rested?"
Emotional: Stress levels, mood, emotional regulation, resilience
- "How would you describe your stress day-to-day?"
- "How do you typically handle difficult emotions?"
Mental/Cognitive: Clarity, focus, memory, mental fatigue
- "How would you rate your mental clarity?"
- "Have you noticed any changes in memory or focus?"
Social: Relationship quality, connection, loneliness, support
- "Do you feel connected to people who matter to you?"
- "How often do you feel lonely?"
Environmental: Living situation, access to resources, safety, nature exposure
- "Does your environment support your health goals?"
- "Do you have easy access to healthy food and places to exercise?"
Existential: Purpose, meaning, values alignment, life satisfaction
- "Do you feel like your life has purpose?"
- "What gets you out of bed in the morning?"
Integrating Objective and Subjective¶
The power comes from combining both:
Example: Client has perfect blood work but reports low energy, high stress, and loneliness. The objective tests say "healthy," but the subjective assessment reveals what's actually going on, so focus: stress management, social connection, sleep, not biomarkers.
Example: Client has concerning metabolic markers but feels great. The subjective data doesn't override the objective concern, so work on both, and the good subjective health suggests they have resources to draw on.
The scenario: Jennifer, 47, has excellent blood work and good functional test scores. But she tells you: "I don't understand. My tests are fine, but I feel awful. I'm exhausted, stressed, and I don't know why I bother."
What NOT to do:
❌ "Well, your numbers look great! You should feel good about that."
Why it doesn't work: You've dismissed her lived experience because it doesn't match the data.
What TO do:
✅ Take the subjective data seriously. Use Deep Health to find what tests missed.
Sample dialogue:
Coach: "Your numbers looking good and you feeling terrible. Those can both be true. The tests measure certain things, but they don't capture everything that matters. Let's dig deeper. Tell me about the exhaustion."
Jennifer: "I sleep 7 hours but wake up tired. I drag through the day. By evening I'm useless."
Coach: "And the stress?"
Jennifer: "Work is relentless. I'm managing a team through a reorg. I come home and just... scroll until I fall asleep."
Coach: "What about feeling like 'why bother'?"
Jennifer: "I used to love what I do. Now I'm just going through the motions. My kids are grown, my job feels meaningless, I don't know what I'm working toward."
Coach: "So we have sleep that's not restful, chronic work stress, and a sense that the purpose has faded. Those won't show up on blood tests, but they absolutely affect how you feel, and eventually they'll affect those numbers too. Which of these feels most important to address first?"
Key takeaway: Subjective data is data. When numbers and feelings don't match, take both seriously.
[CHONK: Putting It Together]
Putting It Together — Practical Assessment Protocols¶
[CHONK: Putting It Together]
Putting It Together — Practical Assessment Protocols¶
The Assessment Hierarchy¶
Tier 1 (Essential, accessible, actionable):
- VO2 max estimation (Cooper test or step test), free
- Grip strength: ~$30-100 for dynamometer
- Functional movement tests: free
- Deep Health questionnaire: free
Tier 2 (Valuable, may need medical collaboration):
- Basic blood panels (metabolic, inflammatory markers): often insurance-covered
- DEXA scan: $40-400+
Tier 3 (Advanced, limited accessibility):
- Full blood panels: $200-800+
- Biological age clocks: $100-500+
- Full body MRI: ~$2,500+
Start with Tier 1. Every client can do these regardless of budget or location, so build from there based on access and goals.
Assessment Timeline¶
Initial (first 30 days):
- Functional tests (VO2 max estimate, grip strength, movement tests)
- Deep Health questionnaire across all six dimensions
- Review any existing medical test results
Ongoing:
- Grip strength: Weekly tracking
- VO2 max: Every 6 months
- Blood panels: Annually (or per doctor's schedule)
- Deep Health check-in: Quarterly
- DEXA: Annually for body composition; every 2-3 years for bone density
Accessibility Reality Check¶
Not everyone can access everything, so work with what clients have:
Limited budget: Focus on Tier 1 entirely. You can do excellent longevity coaching with just functional tests and Deep Health assessments.
Rural location: Functional tests work anywhere. DEXA and lab access may require travel. Factor that into frequency.
Insurance gaps: Know what preventive care is covered (often basic metabolic panels). Help clients prioritize out-of-pocket spending.
[CHONK: Coaching in Practice - Presenting Results]
Coaching in Practice: Presenting Mixed Results¶
The scenario: David, 59, completed his full assessment. Results are mixed: some encouraging, some concerning.
Results:
- VO2 max: 26 mL/kg/min (below target)
- Grip strength: 70 lbs (good)
- HbA1c: 6.3% (prediabetic range)
- hsCRP: 2.4 (average risk)
- Deep Health: Physical struggling (poor sleep, low energy), Social strong
What NOT to do:
❌ Lead with the concerning numbers and create alarm.
What TO do:
✅ Balance honesty with hope by highlighting both strengths and areas for improvement, and make it actionable.
Sample dialogue:
Coach: "David, your assessment gives us a really clear picture of where you are and what to focus on. I want to walk you through the highlights: both what's working and what we need to address.
Strengths first: Your grip strength is solid at 70 pounds. That tells me your overall strength is in a good place, and strength is protective for longevity. Your social connections are strong too, which research shows is huge for health and lifespan.
Areas to focus: Your VO2 max came in at 26, and we're aiming for 35+. That's our biggest opportunity: VO2 max is the single strongest predictor of longevity, and it's highly trainable. Three months of consistent cardio work will move this.
Your HbA1c is 6.3%, which is in the range where blood sugar control could be better. Your doctor should review this, but from a lifestyle standpoint, we can address this through nutrition and exercise: both improve insulin sensitivity.
Your Deep Health assessment flagged sleep and energy as struggles. That aligns with what you've told me about feeling tired. Improving sleep will help everything else.
Bottom line: We have clear priorities: cardio fitness first, sleep optimization alongside, nutrition adjustments to support blood sugar. And we're building on real strengths. What questions do you have?"
Key takeaway: Lead with strengths, be honest about concerns, end with action. Never just dump numbers on people.
The scenario: Robert, 56, has been working with you for 3 months. He's frustrated. He has only lost 5 pounds. But his functional metrics tell a different story.
[CHONK: Coaching in Practice - Motivating with Functional Progress]
Coaching in Practice: When the Scale Disappoints¶
The scenario: Robert, 56, has been working with you for 3 months. He's frustrated because he has only lost 5 pounds, but his functional metrics tell a different story.
Results:
- Baseline: Grip 55 lbs, VO2 max estimate 22, TUG 12.1 seconds
- 3 months: Grip 68 lbs, VO2 max estimate 27, TUG 9.4 seconds
What NOT to do:
❌ "Well, the scale isn't everything. At least your other numbers improved."
Why it doesn't work: You've dismissed his goal while offering weak consolation.
What TO do:
✅ Reframe what "progress" means for longevity and make the functional gains real.
Sample dialogue:
Robert: "Five pounds in three months. I could've done that by just eating less."
Coach: "I hear your frustration. The scale isn't moving as fast as you'd like. But I want to show you something. Look at what's actually happened to your body."
Robert: "What do you mean?"
Coach: "Your grip strength went from 55 to 68 pounds, that's a 24% increase. Your VO2 max improved from 22 to 27, that's more than 20% better cardiovascular fitness. Your TUG time dropped from 12.1 to 9.4 seconds. You crossed from the 'higher risk' zone into the normal range.
Here's why that matters: these are the metrics that actually predict how long and how well you'll live. Research shows they matter more than the number on the scale. You've gotten functionally younger in 3 months."
Robert: "I didn't realize those numbers had changed that much."
Coach: "Most people don't track what matters. The scale tells you one thing: your relationship with gravity. These tests tell you how your body functions. And your body is functioning significantly better than three months ago. The scale will catch up. But even if it doesn't, these improvements are real wins."
Key takeaway: Functional metrics tell the longevity story better than scale weight, so help clients see what actually matters.
Study Guide Questions¶
-
Why is VO2 max considered the strongest predictor of all-cause mortality, and what's the target for longevity?
-
What are the EWGSOP2 grip strength thresholds, and why do they matter for coaching?
-
Name three functional movement tests that predict mortality. What makes them valuable for coaches?
-
What's the difference between what coaches can say about DEXA results versus what requires medical referral?
-
How do you discuss blood panel results with clients while staying in scope? Give an example.
-
Why is Deep Health assessment important even when objective biomarkers look good?
-
What's the "assessment hierarchy" (Tier 1, 2, 3), and why should coaches prioritize Tier 1?
-
How would you respond to a client who says "I don't want to know my numbers"?
-
A client's scale hasn't moved much, but their functional tests improved significantly. How do you reframe this?
-
What's the difference between screening (what coaches do) and diagnosis (what doctors do)?
Self-reflection questions:
-
Think about your own functional markers: How quickly can you get up from the floor? How long can you hang from a bar? Can you easily stand from a chair without using your hands? What do these tell you about your own aging trajectory?
-
When was your last physical exam or bloodwork? What conversations might you want to have with your healthcare provider about longevity-relevant markers?
Want to go deeper? These supplemental articles explore key topics from this chapter in more detail.
- Understanding Blood Panels for Coaches : Non-diagnostic interpretation guidance
- VO2 Max: The Ultimate Longevity Biomarker : Why it matters and how to improve it
- Biological Age Clocks: What Coaches Need to Know: The promise, limitations, and how to discuss with clients
References¶
-
Lang JJ, Tomkinson GR, Janssen I, et al. Cardiorespiratory fitness as a predictor of mortality: an overview of meta-analyses. British Journal of Sports Medicine. 2024;58:595-609. doi:10.1136/bjsports-2023-107731
-
Lang JJ, et al. Mortality risk reduction by cardiorespiratory fitness level. British Journal of Sports Medicine. 2024.
-
Huang W, et al. Dose-response meta-analysis of cardiorespiratory fitness and mortality. British Journal of Sports Medicine. 2022. doi:10.1136/bjsports-2021-104377
-
López-Bueno R, Andersen LL, Calatayud J, et al. Associations of handgrip strength with all-cause and cancer mortality in older adults: a prospective cohort study in 28 countries. Age and Ageing. 2022;51(5). doi:10.1093/ageing/afac117
-
Oksuzyan A, Demakakos P, Shkolnikova M, et al. Handgrip strength and its prognostic value for mortality in Moscow, Denmark, and England. PLOS ONE. 2017;12(9):e0182684. doi:10.1371/journal.pone.0182684
-
de Brito LBB, Ricardo DR, de Araújo DSMS, et al. Ability to sit and rise from the floor as a predictor of all-cause mortality. European Journal of Preventive Cardiology. 2012;21(7):892-898. doi:10.1177/2047487312471759
-
Cheong CY, Yap P, Gwee X, et al. Physical and functional measures predicting long-term mortality in community-dwelling older adults. Aging. 2021;13(23):25038-25054. doi:10.18632/aging.203756
-
Nude T, et al. Gait speed and all-cause mortality: A systematic review and meta-analysis. European Geriatric Medicine. 2018.
-
American College of Physicians. Balance (10-second One-Legged Stance) and Mortality. I.M. Matters Weekly. 2022.
-
Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age and Ageing. 2019;48(4):601. doi:10.1093/ageing/afz046
-
Gierisch JM, et al. Health Coaching. Comparative Effectiveness Review No. 195. AHRQ. 2017.
-
Holt-Lunstad J, Smith TB, Layton JB. Social Relationships and Mortality Risk: A Meta-analytic Review. PLoS Medicine. 2010;7(7):e1000316. doi:10.1371/journal.pmed.1000316
-
Alimujiang A, Wiensch A, Boss J, et al. Association Between Life Purpose and Mortality Among US Adults Older Than 50 Years. JAMA Network Open. 2019;2(5):e194270. doi:10.1001/jamanetworkopen.2019.4270
Chapter 1.4 complete. Proceed to Chapter 1.5: Scope of Practice and Medical Collaboration.